
Citation: Enei ML. Unusual Presentation of Facial Porokeratosis: Dermoscopic Findings and Evolution. Clin Dermatol J 2017, 2(5): 000126.
*Corresponding author: Maria Leonor Enei, Santiago Polanco 2030 2° floor, of 10. Iquique, CP: 1100000, Chile, Tel: +56973006677; Email: leonorenei@vtr.net
The term porokeratosis refers to a group of genetic dermatoses characterized by the histological presence of cornoid lamellae. Here, we report the case of a 12-year-old female with an unusual facial form of the disease that was restricted to the lower eyelid. We describe characteristic dermoscopic findings of this lesion in two distinct stages of its evolution. In addition, we highlight the diagnostic value of dermoscopy for porokeratosis.
Keywords: Facial Porokeratosis; Lesions; Cornoid lamellae; Lower eyelid; Dermoscopy
Abbreviations: PK: Porokeratosis; PM: PK of Mibelli; DSP: Disseminated Superficial PK; DSAP: Disseminated Superficial Actinic PK; PPPD: PK palmaris et plantaris disseminate; CL: Cornoid Lamellae
IntroductionPorokeratosis (PK) refers to a group of keratoses clinically characterized by annular lesions with raised borders and atrophic centres. These disorders commonly affect the limbs and trunk. The classical types of PK are: PK of Mibelli (PM), disseminated superficial PK (DSP), disseminated superficial actinic PK (DSAP), linear PK, punctate PK, and PK palmaris et plantaris disseminata (PPPD). The main histopathological feature of all these clinical forms of PK is the cornoid lamellae (CL), a column of parakeratinized keratinocytes localized on the border of the lesion. Facial localization is rare [1] and is generally described as being part of disseminated clinical forms. Here, we describe an uncommon case of minimal PK on the face, its dermoscopic findings and report the changes that occurred after 6 months of evolution.
Case ReportA 12-year-old female with no personal or family history of interest, reported an asymptomatic lesion in the left lower eyelid that had been present for 1 year. On clinical examination a papule was observed (6x6 mm) with slightly pigmented borders and erythematous squamous centre (Figure 1a). Dermoscopic analysis (Dermalite 3Gen Dermoscope) showed an annular-shaped lesion that appeared as a whitish ring with external maroon delineation. Similar structures to the border with a meshlike appearance were distributed in the central area and around the eccrine ostium (Figure 1b). These characteristics led us to diagnosis of PK which was confirmed by the presence of CL in the histopathological study (Figure 1c). Treatment with adapalene 0.3% and topical imiquimod were done, but the response was minimal. Six months later the lesion was controlled with dermoscopy that evidenced some changes as multiple maroon dots following the border and a central pink area with several linear and dots vascular structures (Figure 1d). Clinically it remained asymptomatic and isolated.
DiscussionDermoscopy is a non-invasive imaging technique that improves the diagnostic accuracy of cutaneous tumours and inflammatory diseases of the skin.
Dermoscopic findings have been reported for clinical cases of DSAP [2-4] and PM [5,6]. The lesion border is described as a single [4-6] or double [2] whitish line surrounded by maroon pigmentation [3]. This whitish structure is histologically correlated with the CL and the maroon delineation, with the confluence of melanophages localized on both sides but not underneath the CL. The central areas have been described as a hypopigmented scar [3-5] or with diffuse maroon pigmentation [6] that could present multiple maroon dots and vascular structures comprised of red lines and dots.
Although PK pathogenesis is still unknown, studies show an abnormal apoptosis of keratinocyte clones [7] along with a de-regulation in its terminal differentiation. These alterations can be induced by ultra-violet radiation [8], infectious agents, trauma, and immunosuppression, consequently triggering the disease development.
It is currently accepted that totipotent stem cells located in the boundary between abnormal clones and normal epidermal originates the CL, characteristic histological structure of PK. From this point CL migrates peripherally, reachs the ostium and infiltrates surrounding areas. The presence of CL in the eccrine ostium and hair follicles has been evidenced by histopathologic studies [9]. In our first dermoscopy analysis we highlight several white plugs localized in the ostium follicular (Figure 1b). This phenomenon was described by dermoscopy before but by staining the hyperkeratotic areas with India ink [10].
ConclusionIn conclusion, we describe a rare clinical presentation of facial PK, consisting in a unique small lesion in the face, with its clinical and dermoscopical evolution after 6 months of control. We recommend the use of dermoscopy as a valuable diagnostic tool, corroborating clinical findings and furthermore allowing us to understand evolutive phenomenon of this desease.
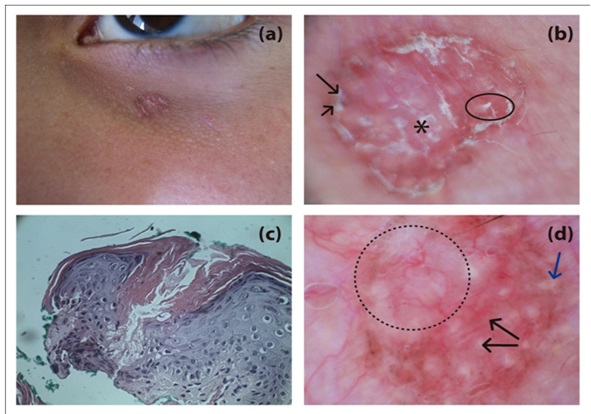
Figure 1A: Clinical presentation: papule 6 x 6 mm in diameter in the left lower eyelid, slightly pigmented border, and erythematous squamous centre.
B: First dermoscopy (10x) (Dermalite 3G). Border: whitish line (long arrow) and maroon-coloured outline (short arrow). Centre: milky white surface with whitish structures surrounding the glandular ostium (asterisk). Several keratotic plugs localized in the ostium (circle).
C: Histopathology (200x): slight acanthosis of the epidermis and hyperkeratosis. Cornoid lamellae comprising a column of keratotic cells in an area of epidermal invagination and absent stratum granulosum.
D: Control dermoscopy (20x) (Dermalite 3G), 5 years later: multiple maroon punctae following the border (short arrow) linear and dots vessels, cicatricial area (circle).