Citation: Elias S, et al. Gastric Twist after Laparoscopic Sleeve Gastrectomy, Diagnosis and Management: A Case Series and Discussion. Diabetes Obes Int J 2017, 2(3): 000159.
*Corresponding author: Elias Saikaly MD, General surgery, Saint George Hospital University Medical Center, University of Balamand, Lebanon, Tel: +9613117869; Email: dreliassaikaly@gmail.com
Obesity is a worldwide endemic, considered nowadays as a disease entity itself. Laparoscopic sleeve gastrectomy is one of the bariatric procedures most commonly used to treat morbid obesity. Like any surgical intervention, bariatric surgeries have their complications. One of the rarest complications of laparoscopic sleeve gastrectomy is gastric stenosis, also known as gastric twist. In this article, we present a case series (6 cases), of gastric twist post laparoscopic sleeve gastrectomy, diagnosed and managed, according to each cause, in our institution, with total symptomatic resolution.
Keywords: Obesity; Sleeve Gastrectomy; Twist; Detwist
Obesity is a worldwide endemic, with an incidence reaching up to 36 percent among adults in the United States [1]. Bariatric surgery is the only effective longterm treatment for morbid obesity, laparoscopic sleeve gastrectomy is an integral part of this surgical treatment [2]. However, Laparoscopic sleeve gastrectomy is not a complication free procedure. Among the complications of sleeve gastrectomy are gastric fistula in 2.5 percent of cases, bleeding in 5 percent and gastric stenosis in 0.69 to 3.5 percent of cases [2]. Currently, gastric stenosis is classified as functional and organic [3]. Functional stenosis is also called gastric twist. Gastric twist can be further classified depending on the timing of its diagnosis into intraoperative diagnosis, early postoperative and delayed postoperative diagnosis.
Case 1EA 21 year old male, with abody mass index (BMI) of 40.8 kg/m2 (125/1.75) presented for sleeve gastrectomy as treatment for morbid obesity. Intraoperative the Boogie used was 34 French. Gastric twist was noted intraoperatively at the level of the incisura angularis and managed by gastroplasty whereby the stomach was incised along the longitudinal axis, incorporating the entire length of the stenotic segment, the incision is then closed in the transverse axis. UGI was done day 2 post operation showed no leak or stenosis. No postoperative complications were encountered.
Case 2TK 67 year old male patient known to have HTN and DMII on medical management with a BMI of 39.4 kg/m2 (125/1.78) presented for sleeve gastrectomy for management of his obesity. Intraoperative the Boogie used was 34 French. Gastric twist was noted intraoperatively at the level of the incisura angularis and managed by gastroplasty whereby the stomach was incised along the longitudinal axis, incorporating the entire length of the stenotic segment, the incision is then closed in the transverse axis. UGI was done day 2 post operation showed no leak or stenosis. No postoperative complications were encountered.
Case 3NA 32 year old male with BMI of 40.8 kg/m2 (114/1.67) transferred to our institution 1 month post sleeve gastrectomy for persistent fever, and dysphagia. Investigated by gastroscopy showing convergence of gastric folds, Upper GI swallow showing dilated esophagus and no passage of contrast distal to the stenosis. Ct scan Abdomen pelvis was in favor of gastric volvulus in the longitudinal axis with a collection near the stapler line. Patient was managed by conversion of the sleeve gastrectomy to Roux-en-Y Gastric Bypass. Intraoperative a stenosis was noted along the incisura angularis and abscess formation near the stapler line. UGI was done day 2 post operation showed no leak or stenosis (Figure1). No postoperative complications were encountered.
Case 4CF female patient status post sleeve gastrectomy 3 months prior to presentation, presented with refractory vomiting, GERD, and dysphasia to solids and liquids. Investigated by gastroscopy which was normal except for hiatal hernia. UGI series done showing esophageal dilatation, reflux of contrast material and stenosis at level of incisura angularis with delayed passage of contrast material. Patient was managed by conversion of sleeve gastrectomy to mini bypass. UGI was done day 2 post operation showed no leak or stenosis (Figure2). No postoperative complications were encountered.
Case 5EA 28 year old male patient with BMI of 44.56 kg/m2 (146/1.81) presented for sleeve gastrectomyfor management of morbid obesity. During surgery no complications were encountered. Day 1 post operation patient reported increased salivation, persistent episodes of vomiting of small quantities of salivary and gastric content every 5 to 10 minutes. Upper GI series was done showing dilated esophagus with stasis of contrast in the distal esophagus and stenosis at level of the mid gastric tube. Patient was managed by conversion of sleeve gastrectomy to Roux-en-Y gastric bypass. Intraoperative a gastric twist was noted at the level of incisura angularis. UGI was done day 3 post operation showed no leak or stenosis. No postoperative complications were encountered (Figure 3).
Case 6MK 32 year old female patient status post sleeve gastrectomy 4 months prior to presentation for management of morbid obesity BMI (39.6 kg/m2) presented with post prandial vomiting of undigested food, and persistent GERD. Investigated by endoscopy showing narrowing at level of incisura angularis and dilated esophagus. UGI series done showing narrowing of the midportion of the gastric tube with dilated esophagus and stasis of contrast proximal to the stenosis (Figure 4). Patient was managed by conversion of the gastric sleeve to Roux-en-Y gastric bypass. Intraoperative axial twist of the stomach was noted on a prepyloric breed. UGI was done day 3 post operation showed no leak or stenosis. No postoperative complications were encountered (Figures 4 & 5).
DiscussionGastric twist is classified depending on the timing of its diagnosis into intraoperative diagnosis, early postoperative and delayed postoperative diagnosis. Patients with functional stenosis can present with a spectrum of symptoms depending on timing of stenosis. In early postoperative diagnosis patients complain of increased salivation and continuous refractory nausea and episodic vomiting of small amounts of saliva and gastric contents. Delayed presentation is manifested by Dysphasia, GERD refractory to medical treatment, vomiting of undigested food and dumping syndrome. Gastric twist can be diagnosed by upper GI series and endoscopic studies after clinical suspicion. During endoscopy convergence of mucosal folds is noted. The Upper GI in the early postoperative period shows delayed passage of contrast, reflux of contrast and dilated proximal stomach and distal esophagus. Whereas during the delayed presentation the Upper GI shows dilated esophagus, stasis of contrast in the esophagus and reflux of contrast. Twisting may occur due misalignment of the staples on the anterior and posterior planes leading to intraoperative diagnosis. Delayed adhesions in the gastric serosa, indentation of the incisura within the gastric lumen which produces a flap valve leading to delayed presentation [2]. The literature mentions that anatomic stenosis can be produced by sharp angulations of the stapler, reinforcing sutures placed over the staple line, a bougie size that is too small, or hematomas and edema [3,4]. Management of gastric stenosis depends mainly on timing of diagnosis. If gastric twist is diagnosed intraoperative then it can be repaired by stricturoplasty, seromyotomy with omental flap, or conversion into Roux-en-Y gastric bypass or mini bypass [5,6] . On the other hand, delayed presentation can be managed by endoscopic dilatation, surgery alone, and surgery after failure of endoscopic treatment. Endoscopic dilatation can be attempted three times before surgical management [5]. In the surgical management approach options are Roux-en-Y gastric bypass, strictureplasty whereby stricture is incised along the longitudinal axis, incorporating the entire length of the stricture, the incision is then closed in the transverse axis, whereas for long stenosis laparoscopic seromyotomy can be done [2]. Some authors also report the possibility of gastrogastric anastomosis after resection of the stenotic segment.
ConclusionGastric stenosis is a rarely reported complication post sleeve gastrectomy with an incidence reaching up to 3.5 percent. Its management is case-based mainly depending on the timing of diagnosis, and requires a multidisciplinary approach including endoscopic intervention and or surgery.
Informed Consent StatementInformed consent was obtained from all individual participants included in the study.
Statement of Humans and Animals RightsNo human or animals rights were violated in this study.
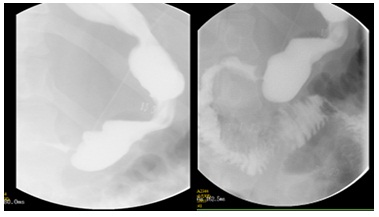
Figure 1: Case 3: Upper GI series (left) did showing gastric twist at the level of the incisura angularis, and another one (right) after management with Roux-en-Y gastric bypass.
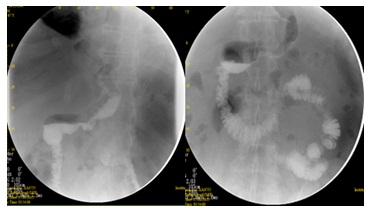
Figure 2: Case 4: Upper GI series (left) done showing gastric twist at the level of the incisura angularis, and another one (right) after management with mini bypass..
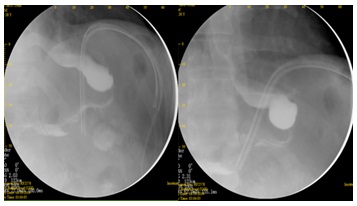
Figure 3: Case 5: Upper GI series (left) done showing gastric twistat the level of the incisura angularis, and another one (right) after management with Roux-en-Y gastric bypass.
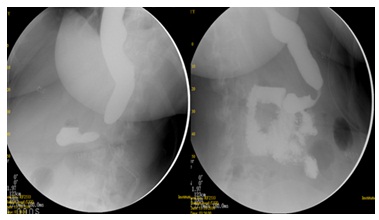
Figure 4: Case 6: UGI series done showing narrowing of the midportion of the gastric tube with dilated esophagus and stasis of contrast proximal to the stenosis.
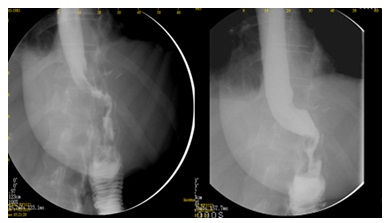
Figure 5: Case 6: Upper GI series after management with Roux-en-Y gastric bypass.