
Citation: Sudarshan RL, et al. Role of CT Mastoids in the Diagnosis and Surgical Management of Chronic Inflammatory Ear Disease. Otolaryngol Open Access J 2016, 1(8): 000144.
*Corresponding author: Sudarshan RL, Department of ENT, Government Medical College, India, Email: drlsudarshanreddy9@gmail.com
Introduction: Chronic Suppurative Otitis Media (CSOM) is a chronic inflammation of middle ear cleft. It presents with discharging ear and decreased hearing. The diagnosis is mostly on clinical examination with otoscope or otoendoscope. Computerized Tomography (CT) of mastoids is done to evaluate the extent of the disease and its complication. High resolution CT is now the investigation of choice for temporal bone disease. This study emphasizes on the importance of CT scan in diagnosis of inflammatory ear diseases and most importantly identifying pitfalls or complications which a surgeon can come across during surgery.
Objectives of the Study: The aims and objectives of this study is:
Results: In this study, 64% of the patients were male and incidence of CSOM with patients undergoing surgery belonged to the age group 21-30 years (32%). The most common presenting symptom was ear discharge (92%) and decreased hearing (96%). The most common type of pathology in this study was attic perforation (36%) and granulations (40%) followed by cholesteatoma (36%) and mucosal edema (16%). Not all cases presented with complications, facial palsy (12%) and mastoid abscess (8%) were among few complications seen. 14 patients (56%) of 25 cases underwent simple cortical mastoidectomy followed by 9 cases (36%) for modified radical mastoidectomy and atticotomy for 2 cases (8%). CT scan findings correlated well with surgical findings for cholesteatoma, middle ear mass and bone erosions. Whereas for ossicular integrity and facial canal dehiscence, there was a discrepancy
Keywords: Computerized Tomography; Temporal bone; Cholesteatoma; Ossicular integrity; Granulations; Facial canal dehiscence
Chronic Otitis Media is a chronic inflammation within the mucosa of the middle ear cleft with varying degrees of edema, submucosal fibrosis, hypervascularity and infiltration with lymphocytes, macrophages and plasma cells. Middle ear cleft include the eustachian tube, hypotympanum, mesotympanum, epitympanum, aditus and mastoid air cell system [1]. There are two types of CSOM- tubotympanic and atticoantral. To know the severity and extent of the disease and to know anatomical variations or destruction/erosions and thence to avoid any complications during surgery, a CT scan of the temporal bone is must to proceed any further with the diagnosis and management of ear diseases. The CT system was invented in 1972 by Godfrey New bold Hounsfield of EMI Central Research Laboratories using X-rays. Allan McLeod Cormack of Tufts University independently invented the same process and they shared a Nobel Prize in medicine in 1979 [2]. There are 4 generations of CT scanners. Modern multi-detector, multi-row CT systems can complete a scan of the chest, for example, in less time than it takes for a single breath hold and display the computed images in near real time. Images that used to take hours to acquire and days to process are now accomplished in seconds. The number of cross sectional images that can be produced has increased from about a dozen to many hundreds [3-10].
Patients and MethodsPatients with suspected middle ear disease attending our outpatient department of ENT at Govt. ENT Hospital, Hyderabad from 2013 to 2014 were included in the study group.
a. Sample size: A total no. of 25 patients has been included in the study.
b. Type of Study: Prospective Study.
Inclusion Criteriaa. Atticoantral type of disease.
b. Any age with unsafe type of disease, both adults and children.
c. Both males and females.
d. Patients with CSOM complications both intra and extracranial Complications.
e. Patients giving consent to undergo CT scan and surgery.
Exclusion CriteriaPatients excluded were:
a. Tubotympanic type of csom
b. Revision cases
c. Bilaterality of disease
MethodologyAll 25 patients included in the study had been explained about the study, need for them to undergo CT Mastoids preoperatively and need for surgery and follow up. Patients were selected randomly initially, then included or excluded based on the criteria listed above. Males, females and children were included in the study done. Lowest age being 7 years in my study all patients included first underwent otoendoscopy to rule out tubotympanic type of chronic ear diseases and also to exclude other pathologies which causes discharging ear like otitis extern a and otomycosis. Patients with active squamosal type or atticoantral type were included after confirming the findings in endoscopy of the ear. Consent for undergoing CT scan and followed by appropriate surgery were taken in written. All basic hematological examinations done for surgical fitness of the patients.
All patients were subjected to CT scan of temporal bone, high resolution in both axial and coronal settings (supine and prone axis) with 1.5 mm thick slices. Scanning commenced from the lower margins of external auditory meatus and extends upwards from the arcuate eminence of the superior semicircular canal as seen on the lateral tomogram. Slight extension of the head was given to avoid the gantry tilt and thereby protect the lens from radiations. Coronal images were obtained perpendicular to the axial plane from the cochlea to the posterior semicircular canal. A radiologist was assigned to read and report all these scans. Surgeries according to the pathology were undertaken, mostly under local anaesthesia, 9 patients underwent GA mostly because of their age. All 25 patients underwent mastoidectomies, postaural approach and graft used was temporalis fascia in all. Simple cortical mastoidectomies in 14 patients modified radical mastoidectomies in 9 patients and atticotomy in 2 patients. On table, the surgical findings were noted in a proforma made exclusively to note down all surgical and radiological findings. These surgical findings were correlated to the radiological findings seen preoperatively on CT mastoids. The surgical findings were also informed to the radiologist to improve the learning curve. Patients were followed up to success rates of surgeries performed with time to time and a regular follow up until ear becomes dry.
Observations and ResultsThis study of 25 patients is based on the observations made in the cases of chronic suppurative otitis media treated in the Department of ENT and HEAD & NECK Surgery, Govt.ENT Hospital, Hyderabad (Tables 1-15).
Simple Cortical Mastoidectomy was done in most cases, 14 cases, 56%. In case of cholesteatoma extending the middle ear cavity, attic and antrum was present, MRM is the best surgery. Hence in all 9 cases of cholesteatoma, MRM is done. MRM (canal wall down) technique gives good view to remove all the disease, it gives good postoperative hearing, and it reduces the chances of residual disease.
CT findings correlated very well with surgical findings (100%) in cases of cholesteatoma. All cases reported as cholesteatoma in CT were confirmed at surgery.
Cholesteatoma was identified on CT scan film by
a. Evidence of soft tissue density.
b. Low attenuation.
c. Absence of enhancement on contrast.
d. Presence of erosion of bone.
The above table shows that the CT findings of soft tissue density i.e. middle ear mass (polyp, granulations) correlated very well with the surgical findings (100%). Mass may be hypertrophied mucosa or granulations in the middle ear. These can be identified by
a. Abnormal soft tissue density.
b. Enhancement on contrast.
c. Absence of bony erosion.
All reported cases were confirmed at surgery.
Bone erosion is early radiological sign of cholesteatoma. Above table shows that there is 100% correlation between radiological and surgical findings in case of detecting bony erosions. All cases reported in CT were conformed at surgery.
Cases reported as facial nerve dehiscence in CT scan were 2, whereas on surgery there were 3 facial nerve canal dehiscence. Facial nerve dehiscence was better seen in coronal cuts of CT. Overlying soft tissues cause a loss of contrast radiance.
In CT Scan Malleus and body of incus are visualized easily. Stapes and I.S joint are visualized with difficulty. The status of ossicular chain was confirmed in 11 out of 16 cases in this study (68.75%).
DiscussionChronic Inflammatory ear diseases can be safe/tubotympanic orunsafe /atticoantral type of diseases. Or can be said as active or inactive mucosalor squamous type. Safe type of disease with a dry perforation in parstensa generally, but not always causes any complication. But with pathology in the atticarea like granulations and cholesteatoma, only clinical examination is not enough to rule out underlying pathology in temporal bone, which not documented before can lead untoward consequences. Hence radiological investigation becomes necessary to assess the pathology in the middle ear cleft. It also becomes necessary in those patients whose tympanic membrane is not visible due to external ear conditions. It is especially useful in children who do not cooperate or in whom visualization of tympanic membrane is difficult. It becomes imminent to investigate radiologically in the patients with intracranial complications. In the present study, all such patients were subjected to CT scan of mastoid bones. HRCT of Mastoids has a capability of displaying all the anatomical structures demonstrated by conventional tomography plus many other structures by virtue of projection advantage and superior contrast resolution [11,12]. This contrast resolution permits the demonstration of soft tissue masses, which is frequently not possible with conventional tomography. Hence, CT imaging is an accurate method of depicting the extent & nature of disease in CSOM. The increased information about disease extent provided by routine CT imaging in all patients with CSOM would assist in-patient counseling, planning the surgical approach and prepares the surgeon for difficult situations.
In the present study we observed
i. The presence and extent of abnormal soft tissue opacity.
ii. Status of the ossicular chain.
iii. Erosion of tegmen or dura.
iv. Facial nerve dehiscence.
v. Fistula in semi circular canal.
vi. During surgery, operative findings are noted.
In the present study, the youngest patient was 7 years and the eldest was53 years old. 8 patients (32%) were in the age group of 21 to 30 years, 5 patients (20%) each in the age groups of 11 to 20 years and 31 to 40 years. Average age of this study comes to 26.28 years, corresponding to the study of [13]. Studies from other countries shows an average age about 35.1 years as in [14]. This variation is due to greater incidence of CSOM cases in children in our country. Male: female ratio was 1.77:1, more for males in accordance with the study done by Vlastarakos, et al. [15] 98% of the patients belonged to low socioeconomic class leading to poor nutrition and lack of hygiene (less in developed countries) [16].
The most common presenting symptom was otorrhea (92%) and hearing loss (96%) followed by tinnitus (76%). Left ear discharge in 56% and Right ear discharge in 44% as shown. Facial palsy was seen in 3 cases, mastoid abscess in 2 cases and labyrinthitis and sigmoid sinus thrombosis 1 case each. Tympanic membrane examination showed attic perforation in 9cases (36%). Subtotal perforation in 5 cases (20%). Marginal perforation in 3cases (12%). Retraction pockets seen in 8 cases (32%). Polyps obscuring view oftympanic membrane was seen in 2 cases. Middle ear pathology included cholesteatoma in 9 cases, polyps in 2 cases, granulations in 10 cases and mucosal edema in 4 cases as shown. 56% of the patients underwent simple cortical mastoidectomy, 36% underwent modified radical mastoidectomy and 8% underwent atticotomy with simple mastoidectomy. MRM is an effective method to manage cholesteatoma in a single staged procedure [17]. Cases those had cholesteatoma underwent MRM for complete clearance. Mastoid cavities healed well after regular follow ups in 84% of the patients. Correlating the radiological and surgical findings- Mastoid bone was sclerotic in all 25 cases. CT scan has 100% sensitivity and specificity to know the type of mastoid pneumatization.
CholesteatomaIn the present study, CT has 100% sensitivity and 90% specificity for diagnosing cholesteatoma through CT images which is in correlation with the studies of Sirigiri & Dwaraknath [18]. It has less sensitivity for cholesteatoma in antrum and aditus where as 100% sensitivity for cholesteatomas in epitympanum and hypotympanum.
Cholesteatoma was identified on CT scan film by
1) Evidence of soft tissue density.
2) Low attenuation.
3) Absence of enhancement on contrast.
4) Presence of erosion of bone.
All cases reported as cholesteatoma in CT were conformed at surgery. The appearance of abnormal soft tissue opacity associated with bone erosion is highly suggestive of cholesteatoma and absence of erosion mostly excludes the cholesteatoma. The purpose of scanning is to know the extent of the lesion. The diagnosis of cholesteatoma in CT is based on the identification of a sharply demarcated soft tissue mass in the middle ear and bony destruction. Inflammatory diseases of middle ear except cholesteatoma was made out by the absence of erosion of otic capsule or ossicular chain, correlated with the studies done by DW Johnson, et al. [9] and found that the presence of a well-defined edge to the soft tissue mass and erosion of otic capsule or ossicular chain were a sure indication of a Cholesteatoma [19] reported a high false positive and false negative rate in pre operative CT scan and suggested that detection rate were dependent on the anatomical site of the disease. This study has achieved 75% results. Wright (1990) - suggested that the ability of MRI in detecting soft tissue changes in cholesteatoma is superior to the CT scan. This study has achieved 90% results. In the present study using the criteria stated above for the diagnosis of Cholesteatoma an accurate assessment could be made out in 100% of the cases. However the suggestion given by [20] that the diagnosis of Cholesteatoma on CT especially in patients with intact tympanic membrane as in Congenital Cholesteatoma and Combined Approach Tympanoplasty and residual disease in the sinus tympani and the facial recess is valuable.
Soft Tissue MassPresent study: HRCT was 84% sensitive and 88.8% specific in identifying soft tissue mass [20] and O'Reilly et al. [19] have similar results, whereas Jackler, et al. [20] and Garber & Dort [8] found it to be less sensitive and specific. However, HRCT is less sensitive in differentiating cholesteatoma from granulations. Mafee, et al. [7] suggested CT scans were able to detect soft tissue masses in the mastoid and middle ear in almost all cases, although he believed it was possible to identify cholesteatoma by its characteristically low attenuation values [21] are of the opinion that Cholesteatoma to be present in 80 of the case explored when bone erosion was present in association with soft tissue density on CT.
Bone ErosionBone erosion is early radiological sign of cholesteatoma. Present study: All cases (100%) reported in CT were conformed at surgery. HRCT detected scutum erosion accurately in all cases. Hence, HRCT is 100% sensitive and specific to detect scutum erosion as per this study. This is in accordance to study by Rocher, et al. [22] but contrasts with study by Vlastarakos, et al. [15], where no correlation was found. Best seen in axial sections; the tegmen slopes downward anteriorly and is not well visualized in coronal sections. Erosion of the posterior wall of the mastoid and the sinus plate occur in extensive Cholesteatomas and may lead to septic Thrombophlebits of the lateral sinus and cerebellar abscess formation [21] detected tegmen erosion in 5 out of 11 cases there was false positives, mainly used axial scans to detect the bony erosion. They stated that it is not possible to reliably demonstrate a dehiscence in the tegmen on axial cuts alone, but even on using coronal cuts they found the effect of partial volume averaging giving rise the false impression of a defect. HRCT detects bone erosion in the middle ear cleft which includes scutum, tegmen tympani, tegmenantri, sinus plate and outer cortex of the mastoid process. Pre operative information of bony erosion gives the surgeon a head on for planning the surgery.
Sigmoid Sinus ThrombosisIn the present study, there was only 1 patient which showed sinus plate erosion. Being small sample size of the study, the results were not in accordance to any study. Other reference study for sinus plate erosion is the patient presented with vomiting, giddiness and an episode of seizure. On CT mastoid, there was soft tissue attenuation indicating cholesteatoma.
Facial Canal DehiscenceFacial nerve canal can be eroded by cholesteatoma, the facial nerve dysfunction occurs in approximately 1% of patients with cholesteatoma. Most facial nerve dehisences occur at horizontal part and this part was clearly seen on coronal cuts. Mastoid segment erosions are best seen in sagittal and coronal sections. However sometimes overlying soft tissues cause a loss of contrast gradience resulting in difficulty to comment on the facial nerve condition. Facial nerve dehiscence was better seen in coronal cuts of CT. Overlying soft tissues cause a loss of contrast radiance. In the present study -- CSOM with facial nerve palsy was seen in 0.08% cases. Whereas CT showed facial canal dehiscence in only 0.12% patients. This is much less than incidence seen by Magliulo, et al. [21] in their study where it was 27% [20-22]. In many cases reported that loss of contrast radiance due to overlying soft tissue obscured a small dehiscence in facial canal are of the opinion that Radio surgical correlation is poor in relation to Facial nerve assessment on CT study.
Ossicular ErosionOssicular erosion was seen in 64% of the cases recorded in this study. Incus was the most common estossicle to be involved. Incus was seen to be eroded in almost all cases of cholesteatoma, [23] followed by stapes and malleus, in accordance with the findings of [24]. In CT Scan Malleus and body of incus are visualized easily. Stapes and I.S joint are visualized with difficulty. Most of the middle ear pathologies appear as soft tissue attenuation on HRCT [25,26], resulting in nonvisualization of the ossicles. In the study, the radiological predictions were compared with the operative findings in each case. This form of imaging (CT) proved to be highly accurate in depicting the extent of soft tissue within the middle ear cleft and mastoid. With the exception of the long process of the incus and the stapes superstructure, the state of the ossicular chain was correctly predicted in over 90% of cases. Erosion of the labyrinth was clearly depicted in 4 of the 5 cases in which it occurred. A correct pathological diagnosis was made radiologically in 88% cases. The selective use of this modality in the evaluation of patients with chronic suppurative otitis media is valuable [27] were able to predict the state of ossicular destruction in only seven percent of cases doubted that CT could demonstrate the ossicular chain reliably because of the combination of partial volume averaging and tissue silhouetting 50% results were achieved in this study.
Congenital CholesteatomaIn the present study, 2 cases of congenital cholesteatoma are included out of 25 cases (8%). Congenital cholesteatoma is difficult to differentiate from acquired type, but clinical features may help; this is commonly seen in children with intact tympanic membrane and absence of previous otologic disease. In our study, one case was of 7 year old female and another 52 year old presenting at first with generalized symptoms of sinus thrombosis. On HRCT, a well circumscribed soft tissue mass seen in antrum and sigmoid sinus plate erosion seen. Congenital cholesteatoma appears as wellmarginated expansile hypodense lesion. Differentiating them by imaging alone is difficult, but history and molecular biological techniques are helpful in differentiating them [28].
Appropriate projections for ossicles and various middle ear structures: The human temporal bone is an extremely complex structure. CT scanning has proved to be the diagnostic imaging method of choice for studying the normal and pathologic details of the temporal bone [29]. CT of the temporal bone should always include at least two projections [30]. The use of a single projection may lead to serious mistakes, since structures parallel to the plane of section are seen only partially or not at all. The basic projection is of course the direct axial (horizontal) plane, since this is the most suitable and practical as well as the easiest projection to obtain for the baseline study of the temporal bone [12,31] . Direct coronal sections can be obtained with many scanners; however, direct sagittal sections are hard or impossible to obtain because of the limitations of the CT scanners [21]. In his study, it is stated that axial scans are more satisfactory as they depict LSSC in its entirety and are less likely to produce false positives. Nevertheless, useful information can also be obtained from coronal scans and hence both sections should be employed. In acute mastoid infection CT scan shows, diffuse opacification of the middle ear and mastoid air cells without evidence of bone resorption. In cholesteatoma the CT appearance is lateral attic wall erosion. The extra dural abscess can occur when pus collects between the dura and bone, which becomes later thickened and covered with granulation tissue. This thickening is seen on a CT as an irregular enhancement. A few minutes discussion with the radiologists about the images demonstrating the course of the facial nerve, the relationship of the inner ear and the condition of the ossicles can be of great help in pre operative counseling and also helps in avoiding the hazards during surgery. The same information discussed with the radiologist improves his/her learning curve.
Conclusion and Summary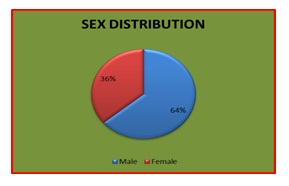
Figure 1: Sex Distribution.
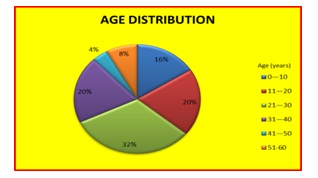
Figure 2: Age Distribution (Total no of cases 25).
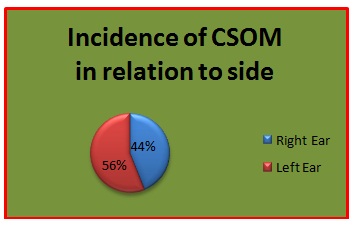
Figure 3: Incidence of Csom In Relation To Side (Total no of cases 25).
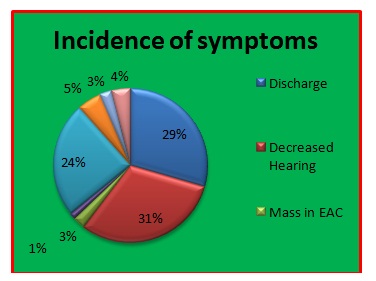
Figure 4: Incidence of Symptoms (Total no of cases 25) Otorrhea and decreased hearing had been most common complaints.
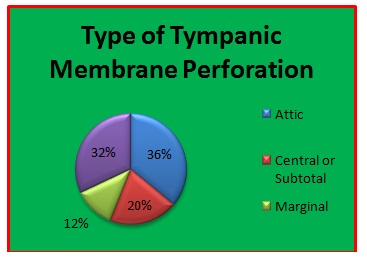
Figure 5: Type of Tympanic Membrane Perforation.
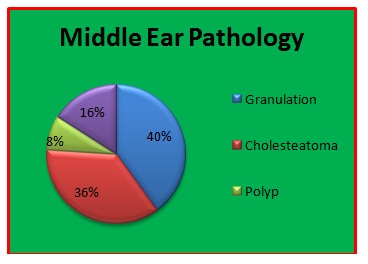
Figure 6: Middle Ear Pathology.
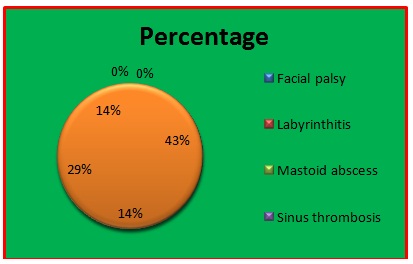
Figure 7: Complications of Csom.
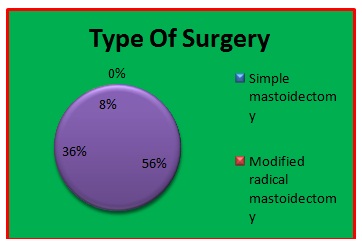
Figure 8: Type of Surgery.
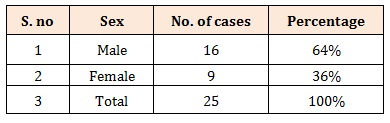
Table 1: Sex Distribution.
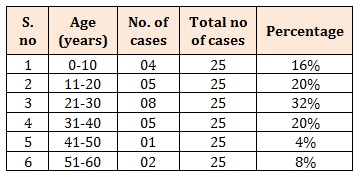
Table 2: Age Distribution (Total no of cases 25).
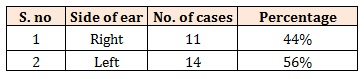
Table 3: Incidence of Csom In Relation To Side (Total no of cases 25).
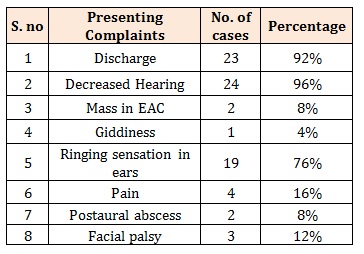
Table 4: Incidence of Symptoms (Total no of cases 25) Otorrhea and decreased hearing had been most common complaints.
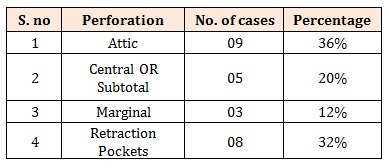
Table 5: Type of Tympanic Membrane Perforation.
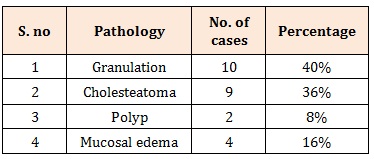
Table 6: Middle Ear Pathology.
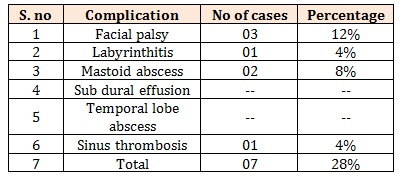
Table 7: Complications of Csom
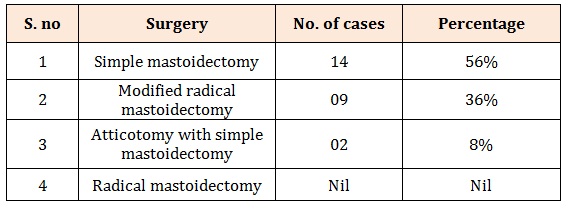
Table 8: Type of Surgery.
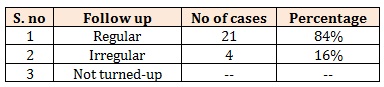
Table 9: Follow Up Records (Total no of cases 25).
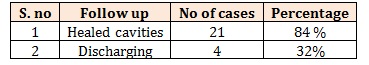
Table 10: Results after 3 Months (Total no of cases 25) In Comparison To CT scan.
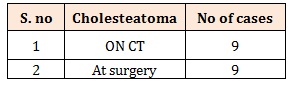
Table 11: Cholesteatoma (Total no of cases 25).
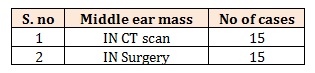
Table 12: Middle Ear Mass (Total no of cases 25).
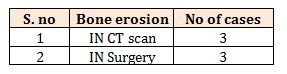
Table 13: Bone Erosion (Total no of cases 25).
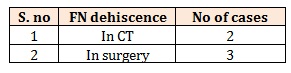
Table 14: Facial Nerve Dehiscence (Total no of cases 25).
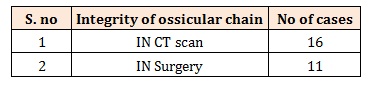
Table 15: Ossicular Chain Integrity (Total no of cases 25).