Citation: Tavares MCM, et al Adductor Pollicis Muscle Thickness as an Anthropometric Parameter in Surgical Patients. Gastroenterol Hepatol Int J 2016, 1(1): 000106.
*Corresponding author: Mayara C.M. Tavares, Master in Biology Applied to Health, Laboratory of Immunopathology Keizo Asami, Av. Professor Moraes Rego, Campus Universitário, s/n, 50670-901 Tel: + 55 84 98279798; Email: mayaramansur@gmail.com
Background: The Nutritional Status (NS) of surgical patients must be followed during the hospital length due to the risk of these patients develop some degree of malnutrition. A new technique for evaluating the muscle compartment is the assessment of the adductor pollicis muscle thickness (APMT).
Objective: To evaluate the APMT as a parameter for assessing NS in pre-surgical patients and compare it with other traditional measures of nutritional assessment.
Methods: Case-series involving 107 adult and elderly patients with more than 19 years of age, of both sexes, admitted at the Hospital das Clínicas, Federal University of Pernambuco. Data collection was done from March to October 2010. NS was determined by Body Mass Index (BMI), APMT of the dominant (DAPMT) and non-dominant (NDAPMT) hands and the adequacy percent of arm circumference (AC), triceps skinfold (TSF), arm muscle circumference (AMC) and corrected arm muscle area (CAMA). Subjective Muscle Assessment (SMA) was applied on the same day of the anthropometric collect.
Results: For the indicators AMC, CAMA, DAPMT and NDAPMT, the most of the individuals were eutrophic. Malnutrition was most often detected by TSF (42.1%). In SMA, there was a significant agreement between the changes of the adductor pollicis muscle and the objective APMT. There was a positive statistical correlation in all the classical anthropometric variables and APMT.
Conclusion: The APMT was as a direct, easy, low cost, safe and reliable method in assessing the NS of surgical patients.
Keywords: Anthropometry, nutritional assessment, nutritional status, general surgery.
Abbreviations: NS: Nutritional Status; APMT: Adductor Pollicis Muscle Thickness; BMI: Body Mass Index; AC: Arm Circumference; TSF: Triceps Skinfold; AMC: Arm Muscle Circumference CAMA: Corrected Arm Muscle Area; SMA: Subjective Muscle Assessment
IntroductionSurgical patients are constantly at risk of developing some degree of malnutrition due to the extensive surgical procedure, which induce physiological changes caused by tissue damage, ischemia and hemodynamic disturbances Such physiological changes, known as acute phase reaction, are characterized by complex metabolic changes. In patients exposed to low and moderate surgical trauma and without complications, metabolic changes are limited, however, in those patients, undergoing major and complicated surgery, acute phase reaction is more pronounced and leads to an increased catabolism and progressive loss of weight and body mass [1]. In these surgical individuals, malnutrition adversely affects clinical outcome, increasing the incidence of infections and postoperative complications, the hospital length and mortality [2].
To determine the nutritional status (NS), a variety of methods can be used. However, a gold standard technique does not exist; hence, nutritional evaluation must be performed using a multivariate approach [3].
Unfortunately, the diagnostic criteria of the NS have important limitations, including edema, lack of standards for the Brazilian population, extremes of age and weight, acute illness, the patient's activity, the high cost and unavailability of appropriate equipment [4].
A new technique for evaluating the muscle compartment is the assessment of the adductor pollicis muscle thickness (APMT), which is simple, non-invasive, fast and presents low cost [5]. Few authors have standardized measures of APMT for healthy individuals [5] and hospitalized patients [6,7] and the literature is still scarce, especially regarding the use of this technique for assessing the NS of surgical patients. Thus, this study aimed to evaluate the APMT as a parameter for assessing NS in pre-surgical patients and compare it with other traditional measures of nutritional assessment.
Materials and MethodsCase-series conducted with adult and elderly patients of both sexes admitted at the surgical ward of the Hospital das Clínicas, Federal University of Pernambuco (HCUFPE), from March to October 2010.
The study excluded patients unable to provide information and who were without companions, unable to be submitted to anthropometric evaluation, applicants for small corrective surgery (otorhinolaryngologic, ophthalmic and plastic), pregnant women, individuals with edema and ascites, amputees and those who have suffered injury or fracture in hands.
Several variables were considered: sex, age, socioeconomic conditions, proposed surgery, clinical diagnosis, comorbidities, and nutritional status. Data collection was done through a form specially designed for this research, operated exclusively by the researcher, containing items for registration regarding the clinical, socioeconomic and anthropometric data.
Nutritional analysisThe assessment of NS by anthropometry was performed in pre-surgical patients within 72 hours after admission. The assessment included weight, height, triceps skinfold (TSF) and arm circumference (AC). The patients were weighed using a Filizola platform balance, with a capacity of 150kg and precision of 100g, and height was measured by stadiometer attached to the balance with a capacity of 1.90m. The body mass index (BMI) was obtained using the WHO classification (2000) [5] for adults and classified according to Lipschitz [8] for the elderly. The measurement of the AC was performed with the arm flexed toward the chest, forming an angle of 90° to mark the midpoint between the acromion and olecranon. With the arm extended along the body, palm facing the thigh, the arm was bypassed with a nonextensible tape measure at the marked point [9]. The TSF was measured with a CESCORF® adipometer, previously calibrated, in the same midpoint used for AC, with the arm relaxed and loose at the side of the body, softly separating the fold of the arm, detaching it from the muscle tissue and applying the calibrator forming a right angle [10]. Three measurements were performed and then it was calculated the average between them. To the consistency of the data were excluded from the measures those that showed differences greater than 1mm. Using the measures of AC and TSF, were obtained the arm muscle circumference (AMC) and the corrected arm muscle area (CAMA). To calculate the CAMA the equations proposed by Heymsfield [11] were applied, and individuals with malnutrition were those in which the measures were below the 15th percentile [9]. To assess the percent of adequacy of AC, AMC and TSF, it was used the 50th percentile of the measures proposed by Frisancho [12] to individuals until 74.9 years, and for individuals over 74.9 years, it was used the 50th percentile of the measures proposed by Burr [13], considering as malnourished the individuals with adequacy less than 90%.
The APMT was assessed with the subject seated with both hands resting on the knee, elbow angle of approximately 90º on the homolateral lower limb. It was used the adipometer CESCORF® with a pressure of 10 g / mm2, to clamp the adductor muscle at the apex of an imaginary triangle formed by the extension of the pollicis and index finger [14]. The measurement was done in both hands, considering the dominant APMT (DAPMT), which was performed in the right hand of right handed patients and left hand of left-handers; and the non-dominant APMT (NDAPMT), which was performed in the left hand of right-handers and right hand of left-handers [5]. The average of three measurements was considered as a measure of the muscle thickness of each hand, and, to the consistency of the data, were excluded from the measures those that showed differences greater than 1mm. The cutoff point used for the diagnosis of malnutrition in both sexes and all age groups was 13.4 mm for the dominant hand and 13.1 mm for the non-dominant hand, proposed by Bragagnolo [15].
Subjective Muscle Assessment (SMA) was applied on the same day that anthropometry was performed using the protocol to detect changes in specific muscle groups: masseter, temporalis, adductor pollicis, interosseous and gastrocnemius. The criteria used for classification was proposed by Lameu [4], which considers the muscle changes as mild, moderate and severe atrophy, or simply the presence or absence of atrophy.
Statistical analysisFor statistical analysis was used SPSS (Statistical Package for the Social Sciences) version 13.0 for Windows and Excel 2003. Continuous variables were tested for normal distribution using the Kolmogorov Smirnov. Numerical variables were represented by measures of central tendency and dispersion measures. The statistical analysis was performed using the "t" student and the verification of possible correlations, between all methods of anthropometric assessment with APMT, was performed using Pearson correlation. In association verification test, it was applied chi-square for categorical variables. To evaluate the correlation between APMT and SMA it was used the kappa index. The results were presented in tables and figures. Significance level was set to 5% for all tests.
Ethical considerationsThe study protocol was approved by the Committee of Ethics Research involving Human beings from the Center of Health Sciences, Federal University of Pernambuco (CEP / CCS / UFPE Registration No. 039/2010). All participants gave their written consent, through the informed consent forms in accordance with the ethical standards, required by Resolution No. 196/October 1996 of the National Health Council [16].
ResultsThe sample comprised 107 patients, where 42 (39.2%) were elderly and 66 (61.7%) of the participants were female. The average age of the group was 53.5 ± 16.2 years, with a minimum of 20 years and maximum of 86 years.
The socioeconomic and clinical characteristics evaluated are presented in Table 1, where it was observed that 48 patients (approximately 46.0%) had completed / uncompleted elementary education, 51 (53.7%) had income per capita from 0.5 to 1,0 minimum wages and 40 individuals (37.4%) were retired, which represents the majority of the sample. As diagnosis, 42 patients (39.3%) were cancer, including gastric adenocarcinoma, pancreatic and esophageal cancers. 52 patients (48.6%) had hypertension, which was the co-morbidity more detected.
The nutritional classification by the anthropometric parameters is shown in (Table 2) y the nutritional indicators AMC, CAMA, DAPMT and NDAPMT the highest percentage of individuals were eutrophic. The malnutrition diagnosis, by the classical parameters, was more found on the TSF, with 45 patients (42.1%), and less observed on BMI, with 16 patients (15%). Regarding the practice of regular physical activity, only 23 (21.5%) of the studied individuals practiced some type of physical exercise.
Of the total patients, 99 were right-handed (92.5%). The average found of APMT, including both sexes, was 15.2 ± 3.9mm for the dominant hand and 14.3±3.8mm for the non-dominant hand. The mean values of the various techniques used to assess the NS of patients according to the cutoff point for DAPMT and NDAPMT are shown in Table 3. It was verified significant difference between mean values of all anthropometric variables.
In SMA it was observed superficial atrophy of the temporal muscle in 63 (58.9%) patients, 44 (41.1%) showed this event in the adductor pollicis muscle, 25 (23.3%) in the interosseous muscles and 32 (29.9 %) in the gastrocnemius muscle.
In relation to the degree of correlation between objective APMT and the muscle disorders of the adductor pollicis, according to the SMA, there was significant agreement (p<0.001) for both hands, with a kappa coefficient of 0.473 for the dominant hand and 0.463 for the non-dominant hand.
Figure 1 & Figure 2 shows a positive correlation (p<0.05) among all the traditional anthropometric parameters with DAPMT and NDAPMT, demonstrating the harmony of this measure with others of NS assessment. The main correlation of the DAMPT (r=0,51) and NDAMPT (r=0,50) was with the TSF.
DiscussionIn the Brazilian Northeast, in particular in the state of Pernambuco, which has a poverty incidence rate of 52.5% [17], is common the unfavorable economic situation of most of the population, reflecting in the individuals admitted to public hospitals that are generally registered in the Brazilian Unified Health System (SUS). In the present investigation, the observed socioeconomic conditions corroborate with the situation found in the State and the country, as well as describes the Brazilian Survey on Hospital Nutritional Assessment (IBRANUTRI) [18], in which 22.6% of the population were illiterate and 47.6% had completed/uncompleted elementary education.
Studies conducted in different countries have shown a high incidence of hospital malnutrition in adults over the years [19]. In Brazil, the IBRANUTRI, multicenter study published in 2001, which assessed the nutritional status of 4000 patients, revealed that 48.1% had some degree of malnutrition [18]. On the present study, similar results were obtained with 42.1% of the population showing malnutrition, more specifically by the TSF, fact that demonstrates the increased specificity of this parameter when attempting to measure the impact of fat mass loss triggered by the disease.
Other studies also obtained similar results, as in Cuba, where it was found that among 12 institutions, 41.2% of the subjects had malnutrition [20]. In a study with 241 patients eligible for elective surgery at a university hospital in Cuiabá - Mato Grosso, 31.5% had some degree of malnutrition [21]. Although the concern data, the situation is getting worse, as shown in a study completed in the same department after 15 years, by the same authors, who found an increase in the percentage of malnutrition which jumped to 41% of patients [22]. Correia & Campos [23], through a multicenter study named Latin American Nutrition Study involving 9348 patients, also had similar values to those found in the present investigation, in which 50.2% had malnutrition.
BMI has been one of the most anthropometric parameter used to identify individuals at nutritional risk, because of its ease of application and low cost [24]. In this study, the use of BMI, as a method to identify malnutrition, this parameter showed a lower percentage (15%) when compared with other evaluation methods. Similar results were also found by Mello [25], Norman [26] and Manzanares [27]. Therefore, as a parameter that provides a measure of all compartments of the body, its use in hospital patients must be limited, since these individuals can exhibit fluid retention, due the fluid replacement, and do not present a real loss weight, underestimating the incidence of malnutrition, when used alone [24,26,27].
In the nutritional assessment of hospitalized patients none of several existing anthropometric methods can be regarded as the gold standard for nutritional diagnosis. It is advisable to use the various available methods, in order to establish the best NS [28,29].
The APMT has been studied as anthropometric measurement because it is located between two bony structures and it is the only muscle that allows a proper assessment of the thickness, and presents well-defined anatomical reference [30]. The first published study with APMT as an anthropometric method evaluated 421 healthy subjects with preserved NS [4]. The average of the individuals of both sexes for the dominant hand was 11.5 ± 2.76 mm, whereas in the present study was 15.2 ± 3.9 mm. This difference can be explained by methodological differences in the study above, which used the Lange ™ adipometer and in the present study it was used the Cescorf ® brand.
The mean of the DAPMT and NDAPMT was respectively 15.2 ± 14.3 ± 3.9 mm and 3.8 mm, fact that agrees with the work of Lameu [7], performed with patients in wards of the Medical Clinic from the Hospital of the University of Rio de Janeiro, that found an average of APMT for the total sample of 14.2 ± 3.7 mm in the dominant hand and 13.8 ± 3.7 mm in the non-dominant hand. However, Freitas [31] in a study with 82 cancer patients at St. Mark's Hospital in Teresina, Piauí, observed a lower average (13 ± 3.2 mm) of APMT for the dominant hand and both sexes.
When evaluating the percentage of nourished by APMT, it was verified 61.7% for the dominant hand and 57% for the non-dominant hand, showing that in preoperative of surgical patients, despite the severity of the underlying disease, the mass and function of the adductor pollicis are maintained while is possible to preserve the labor activity [32,33].
The degree of correlation between objective APMT and the muscle disorders of the adductor pollicis, according to the SMA (p<0.001), reflects a diagnostic reproducibility between the subjective and objective method for evaluating the APMT and confirms that the Subjective methods have good diagnostic accuracy when used by an experienced professional [9].
In this study there was also a significant positive correlation (p <0.001) among all the classic anthropometric parameters with DAPMT and NDAPMT.
Caporossi [34], studying individuals in intensive care, found that the correlation measures of dominant and nondominant APMT were significant when compared to measures of AC, AMA and TSF, which corroborates to the present study. Similar results to this investigation were also found by Rosalie [35], with 124 patients eligible for large digestive surgery hospitalized in the Surgical Clinic of Julio Muller University Hospital, where the APMT of both hands was positively correlated with all anthropometric variables. In contrast, Lameu et al [30], in a study with healthy subjects, found a significant relationship between APMT and anthropometric parameters, but only for those that estimates muscle mass and not between APMT and parameters that estimates fat mass. It is important to point that the mentioned study was not performed in surgical patients, but in healthy subjects.
The limitations of this study were the few numbers of studies regarding the APMT as an anthropometric parameter, and the lack of a cutoff point for the healthy and hospitalized population, especially those patients at surgery wards.
ConclusionIn summary, the APMT showed positive and statistically significant correlation with all the classics anthropometric parameters, showing itself as a direct, easy, low cost, safe and reliable method in assessing the NS of surgical patients. Its use should be associated with clinical, physical and anthropometric data, to enable an adequate nutritional intervention to assist in the recovery and/or maintenance of the NS of the individual.
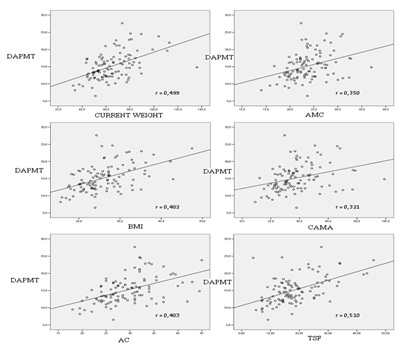
Figure 1: Correlation between DAPMT with anthropometric indicators of individuals hospitalized in surgical wards of the HCPE. Recife, Brazil, 2010.
*Correlation analysis by Pearson's test; ‡ DAPMT=Dominant adductor pollicis muscle thickness
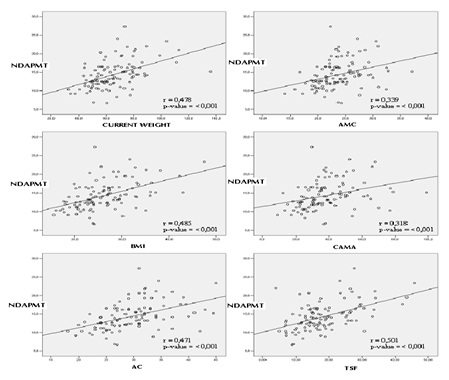
Figure 2: Correlation between NDAPMT with anthropometric indicators of individuals hospitalized in surgical wards of the HCPE. Recife, Brazil, 2010.
*Correlation analysis by Pearson's test; ‡ NDAPMT= Non-dominant adductor pollicis muscle thickness
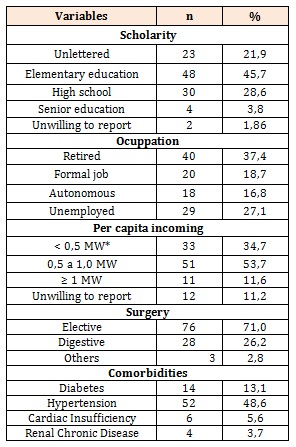
Table 1: Socioeconomic and clinical characteristics of patients hospitalized in surgical wards of HCPE.
*MW: Minimum wage of reference = R$510,00 (US$ 867,00)
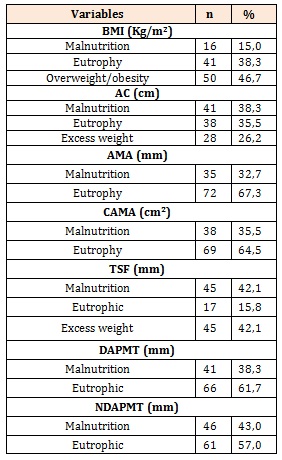
Table 2: Nutritional classification by anthropometric parameters of patients hospitalized in surgical wards of HCPE.
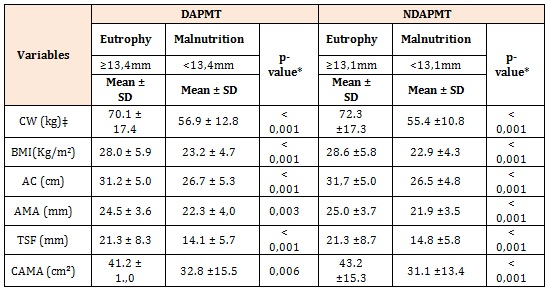
Table 3: Distribution of mean values of classical anthropometric according to the nutritional status determined by APMT of both hands of individuals hospitalized in surgical wards of the HCPE. Recife, Brazil, 2010
* Significant difference at 5.0% through the Student t test; ‡ CW: current weight