
Citation: Ooi M. A Rare Case of Esophagitis Dissecans Superficialis “Sloughing Esophagitis”. Gastroenterol Hepatol Int J 2017, 2(3): 000125.
*Corresponding author: Dr Marie Ooi, Gastroenterology and Hepatology Unit, Royal North Shore Hospital, Reserve Road, St Leonards, NSW 2065, Australia. Contact: 0430669940, Fax: 61294632041; Email: marieooi_al@yahoo.com
Esophagitis dissecans superficialis (EDS) or sloughing esophagitis is a rare idiopathic condition and is often underreported and under-recognized entity. It is characterized by strips of denuded esophageal mucosa with minimal or no bleeding. EDS was first described in 1892, since then, there have been only very few case reports. Herein, we illustrate a case report of this rare entity that may serve to remind us of this often forgotten condition.
Keywords: Slough esophagitis; Esophagitis dissecans superficialis: Desquamated esophageal mucosa; Upper endoscopy; Gastroscopy
Esophagitis dissecans superficialis (EDS) or sloughing esophagitis is a rare, benign cryptogenic condition of the esophagus, characterized by exfoliated superficial esophageal mucosa. Histologically, it is characterized by desquamated superficial epithelium of the esophageal lining. EDS tend to be associated with polypharmacy in elderly debilitated patients [1]. Clinically, majority of patients are asymptomatic. Most EDS are detected in the distal or mid-esophagus, however up to 23% EDS affect the entire esophagus [1]. The etiology of this condition remains unclear, although several exogenous agents such as chemical or corrosive irritants have been implicated to explain the denuded esophageal mucosa suggestive of possible contact injury rather than ischemia. This case report illustrates a debilitating patient who was diagnosed with EDS.
CaseA 68 year-old man with a history of neurodegenerative disease, major depression and malnutrition was admitted with weight loss. He had no prior symptoms of dysphagia, nausea and vomiting. The patient also had no reported skin-related symptoms or associated autoimmune conditions. His regular medications included benzodiazepine, aspirin and multivitamins. Clinically, he appeared frail with no other significant findings. Esophagogastroduodenoscopy (EGD) was performed, which revealed streaks of peeled desquamated esophageal mucosa with circumferential cracks and long linear mucosa break (Figure 1). The lower third of the esophagus revealed clumps of exfoliated esophageal mucosa (Figure 2). Biopsies were taken from the proximal esophagus, histopathology of which was reported as superficial disaggregated epithelium that is entirely separated from the underlying squamous mucosa (Figure 3). These endoscopic appearances were consistent with esophagitis dissecans superficialis (EDS), also known as sloughing esophagitis. The patient was treated with oral proton pump inhibitor (pantoprazole 40 mg daily) for a week. A follow-up EGD showed complete normalization of the esophageal mucosa.
DiscussionEsophagus Dissecans Superficialis (EDS) was first reported in 1892 [2]. It is a rare and benign condition, also known as sloughing esophagitis and is an underrecognized entity whereby its prevalence or incidence rate is largely unknown [3]. EDS is characterized by strips of detached superficial mucosa but can present as vertical fissures, circumferential or long linear mucosal breaks in the esophagus and tends to be associated with minimal or no bleeding [4]. Patients are mostly asymptomatic, but some may report symptom of dysphagia and very rarely, vomit out casts of esophageal mucosa [5][6]. Histologically, there is superficial eosinophilic, necrotic squamous epithelium that is either partially or completely detached from the underlying epithelium. This endoscopic finding is most often seen in debilitated or malnourished elderly patients such as in our patient and who are typically on multiple (at least 5) medications including central nervous system depressants [1]. The pathogenesis is virtually unknown and is most often idiopathic. However, EDS has been linked to various forms of esophageal mucosal injury that includes iatrogenic, chemical, thermal, immunological or allergic reaction. Based on the reported cases linking EDS to nonsteroidal anti-inflammatory, bisphosphonate, consumption of hot beverages, heavy smoking, mediastinal radiation, endoscopic therapy (sclerotherapy, esophageal dilatation and band ligation), autoimmune bullous dermatoses, lichen planus, celiac disease and cardiac disease (valvular or congestive heart failure) [7- 10]. Diseases such as monilial esophagitis, eosinophilic esophagitis (EoE) and corrosive esophagitis may mimic EDS, hence emphasizing the need for esophageal biopsy [2].
Despite the dramatic endoscopic appearance, sloughing esophagitis, complete resolution of mucosal injury is usually achieved without any long-lasting clinical consequences through combination of acid suppression and discontinuation of the precipitating factors and medications. In the setting of bullous dermatoses, steroid therapy may be required for mucosal healing [9].
ConclusionIn summary, EDS remains an enigma to many health professionals where the etiology is largely unknown and is characterize by its dramatic endoscopic appearance and complete resolution with no long-term sequelae.
Conflict of Interest declarationAuthor has no conflict or financial interest related to this article.
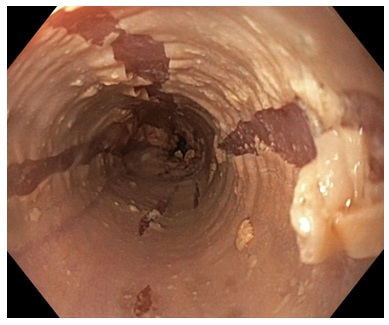
Figure 1: Upper endoscopy revealed the presence of streaks of peeled desquamated esophageal mucosa with circumferential cracks and long linear mucosa break.
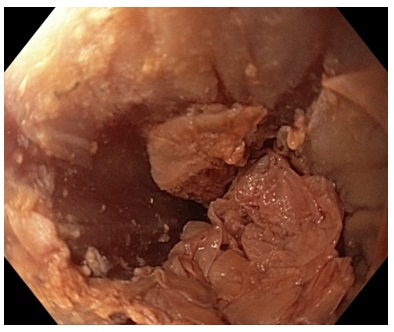
Figure 2: Endoscopic view of the lower third of the esophagus revealed clumps of exfoliated esophageal mucosa.
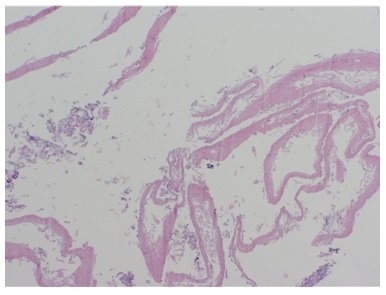
Figure 3: Histology: H & E stain demonstrated strips of superficial disaggregated epithelium of esophageal mucosa.