
Citation: Chia CY, et al. Clinical Anatomy of the Face. Clin Dermatol J 2017, 2(1): 000107.
*Corresponding author: Chang Yung Chia, Av. das Américas, 505 suit 203, Barra da Tijuca, Rio de Janeiro CEP 22.631- 000, Brazil, Tel: 55 21 99649-5164; Email: changplastica@gmail.com
Replacement and redistribution of face volumes is an essential part of facial aesthetic treatment, however, updated concepts of the aging process and the anatomy on which treatment is based are still confused and conflicting in the literature. The authors summarize the updated concepts of the aging process and anatomy, based on recent literature, clinical experience and the author’s fresh cadaver dissection study.
Keywords: Facial anatomy; Facial aging; Tear trough; Nasolabial sulcus
The most recent advances in facial aesthetics treatment were the better understanding of facial natural aging process, and better comprehension of facial anatomy. With this knowledge, aesthetic and reparative facial treatments advanced, both in plastic surgery and in dermatology [1-3]. The present paper summarizes the latest concepts of the aging process and anatomy, and this comprehension may enable increased therapeutic possibilities. It is based on recent literature, clinical experience and the author’s fresh cadaver dissection study.
Unaesthetic CharacteristicsThere is a lot of confusion between rejuvenating and beautifying, and many unaesthetic facial characteristics are not due to aging [1]. The face is formed by the reunion of many organs, the eyes, the nose, the mouth and the ears. Beauty is related not only to each organ feature, but also to their relationship and the harmony of the elements as a whole. Even though these organs are contiguous, they are not continuous, and each organ is an anatomically and functionally independent structure. Each facial region has different skin and subcutaneous tissues from the adjacent areas, with or without underlying muscle, which may also vary in strength and vector. Furrows, folds and wrinkles usually appear at the transitional limits of these anatomical units [2]. For example, the malar region is one aesthetic unit, with rounded and smooth surface [1]. However, anatomically, it comprises three distinct regions: the thin-skinned orbital region over the orbicularis oculi muscle, with sparse subcutaneous tissue; the cheek region with thick skin and subcutaneous adipose compartments on top of the superior lip elevator muscles; and the zygomatic region, of intermediate thickness skin, on top of the subcutaneous adipose compartment, orbicular oculi muscles and origin of the greater zygomatic muscle on the zygomatic bone prominence [1,2,4]. The boundary between the orbital, the nasal, and the buccal regions is the nasolacrimal sulcus. The zygomatic region is separated from the oral region by the buccal zygomatic groove and from the orbital region by the palpebromalar groove [5] (Figures 1 and 2). These characteristics are already present in the youth, butonlybecome more evident with excess skin and with hypertrophy and atrophy of the fat compartments, and with skin aging itself1. The aesthetic treatment consists in making these three anatomical structures in a single homogeneous aesthetic unit, which is of extreme difficulty [1] (Figure 3).
Gravity was thought to cause a lower positioning of anatomical structures, and the "gravitational" theory was created to explain aging. Today, it is known that aging is genetic, not gravitational [6-9]. The skin becomes thinner and atrophic, with less cellular elements, less vascularity, decreased collagen and elastic fibers, flattening of the dermoepidermal papillae, and increased radial extension. Together with variations of the underlying volume, these changes result in grooves, folds and wrinkles [10]. Adipose compartments, which have independent metabolism, become atrophic or hypertrophic, and along with the continuous remodeling of facial bones, alter the shape of the face [8,9].
The change in skin quality and its consequences constitute the major difference between youth and old age, along with the redistribution of volumes caused by altered adipose metabolism [1,3]. There is little muscle alteration in the aging process [11,12].
There is no treatment for genetic, or intrinsic aging [13]. Prevention is the best therapy for extrinsic aging, such as avoiding sun exposure, which is the major external cause of skin aging, smoking, etc. Cell therapy, perhaps the only non-ablative method, such as autologous lipoaspirate grafting, is currently the focus of extrinsic aging treatment research. In fact, researches are still initiating with only slight advances in the process of cutaneous regeneration [14-16]. Ablative methods may, in the long term, cause atrophy, and should be applied with prudence [17]. The most significant results in facial aesthetics are the anatomical ones. The major unaesthetic anatomical changes of the face are illustrated and analyzed (Figure 3).
Nasojugal Groove, Nasolacrimal or Lacrimal Gut (Tear Trough)There is much controversy regarding anatomy, and tear trough is inaccurately thought to be caused by aging. Tear trough is a personal anatomical characteristic, present from childhood [1] (Figure 4).
It is located below the medial canthus of the eye and is directed inferiorly and laterally to a little more than the lateral half of the orbit, a few millimeters below the orbital rim. It is mostly caused by the transition from the thin palpebral skin, devoid of subcutaneous adipose tissue, to the thicker malar skin with underlying subcutaneous tissue [1,18]. A ligament has been described as its cause; however, other authors argue that the ligament is the bone origin of the pre-orbital part of the orbicularis oculi muscle (Figure 5) [19,20]. It may also be accentuated by a bone depression at the muscle origin, anterior to the anterior lacrimal crest [1,2]. In addition to depth variations, the thin skin is further darkened by abundant blood vessels and increased skin pigment (Figure 6) [1].
Palpebromalar GrooveIt can be continuous with the tear trough, or continuity can be interrupted by the V-shaped deformity. It is directed lateral and superiorly, along with, but below the orbital border. It is mainly caused by the difference in the malar adipose compartment, the transition from the palpebral skin to the malar skin, and by the zygomatic bone prominence (Figure 7)[1,2,18].
Buccal Zygomatic GrooveIt begins at the V-shaped deformity, or at the junction of the tear trough with the palpebromalar groove, moving in an inferior and laterally, obliquely dividing the cheekbone (Figure 8) [1,2]. It have several peculiarities: the groove accompanies the convexity of the malar bone in the transition to zygomatic prominence; There is a clear difference in the cutaneous characteristics of the malar region and the region of the nasolabial compartment; And, internally, it is the anterior limit of the oral cavity, which means it is the limit between the mobile part of the cheek and the fixed malar area (Figure 9) [1,2]. The described zygomatic ligament as cause of the sulcus, however, is uncertain [21].
V-Shaped DeformityIt is a triangular depression in the middle region of the inferior orbital border, where the tear trough, the palpebral-malar and zygomatic-buccal grooves meet. It is caused by a lack of adipose tissue between the nasolabial and malar compartments associated to the zygomatic bony prominence (Figure 10) [1,2,5].
Nasolabial grooveIt starts laterally to the nasal wing and is inferior and laterally directed, ending laterally to the modiolus. Sometimes it may join with the lip-mandibular groove (Figure 11). It is caused by the transition of the (redundant) skin of the cheek with the nasolabial adipose compartment, to the labial skin devoid of subcutaneous adiposity and well adhered to the orbicularis oris muscle. The groove demarcates the limit of the orbicularis oris muscle and the insertions of the upper lip elevator muscles and the zygomaticus minor (Figure 12) [1,2].
Labiomental GrooveThis is, perhaps, the most remarkable feature of aging. Usually begins at the corner of the mouth, is directed inferiorly and laterally and it can be continuous with the nasolabial fold (Figure 13), lateral to the modiolus. This crease is formed by the transition between the excess skin along with the subcutaneous adipose compartment of the jowl, laterally, and the lower labial skin firmly adhered to the orbicularis oris muscle and to the depressor anguli oris muscle (Figure 14) [1,2].
Based on current concepts of anatomy and of the aging process, facial aesthetic treatment consists on adipose volume redistribution and contour restoration by rebalancing the existing volume to the amount of skin through redundant skin excision. Improving skin texture and its quality, with less or no ablative methods. For a complete and long-lasting result, it is necessary to combine modern surgical techniques, that cover the upper, middle and lower thirds of the face, with more vertical vectors, and scars extension as required, with cell therapy in volumetric replacement and tissue "regeneration" (Figure 15) [22].
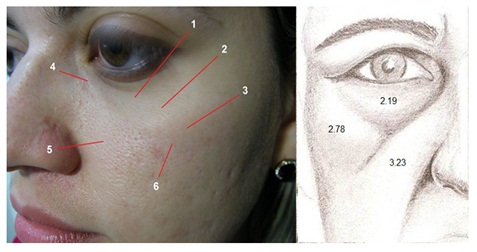
Figure 1: Left: Malar region, containing three different anatomical areas (1) skin of the orbital region, (2) palpebromalar groove (3) skin of the zygomatic region, (4) nasolacrimal sulcus, (5) Skin of the buccal region, and (6) buccal zygomatic groove. Right: Skin thickness in each area, in millimeters.

Figure 2: Aesthetic treatment of the malar area: uniting the three anatomical structures into one homogeneous aesthetic unit. Preoperative of autologous lipoaspirate graft (left); 2 years postoperative (right).
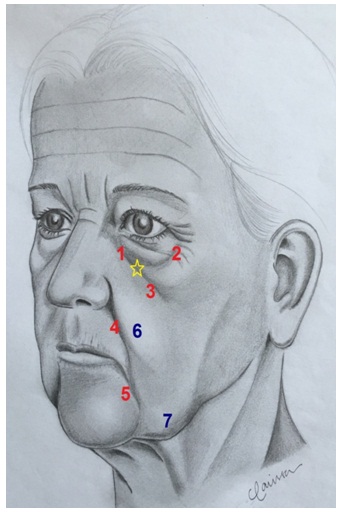
Figure 3: Unaesthetic facial characteristics. (1) nasolacrimal sulcus, (2) palpebromalar groove, (3) buccal zygomatic groove, (Star) V-shaped deformity, (4) nasolabial groove, (5) labiomental groove, (6) nasolabial fat compartment, (7) jowl.
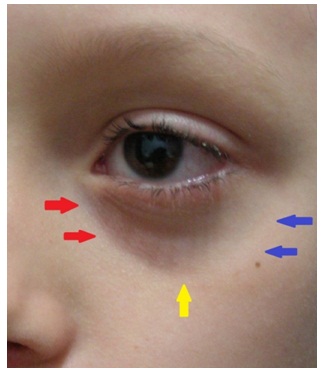
Figure 4: 6-year-old child with nasolacrimal sulcus (red arrows), palpebromalar groove (blue arrows) and Vshaped deformity (yellow arrow).
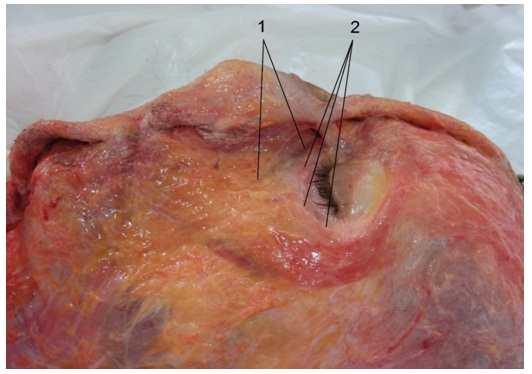
Figure 5: Anatomical dissection in fresh cadaver. (1) Nasolacrimal sulcus or tear trough. (2) Orbital bone rim. Note the presence of adipose compartments below the bone rim.
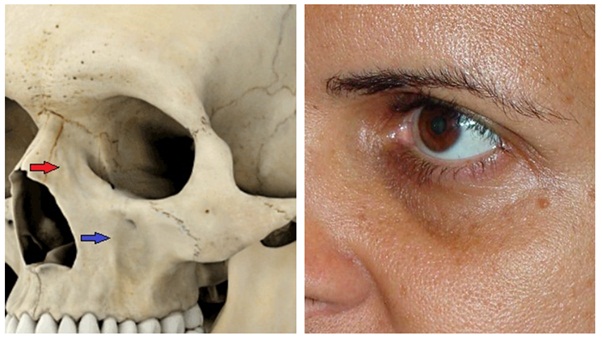
Figure 6: Left: Bone depression in the origin of the orbicularis oculi muscle, pre-orbital segment (red arrow); Concavity of the maxillary bone (anterior border of the oral cavity) (blue arrow). Right: besides depth variations, the skin is thin and hyperpigmented.
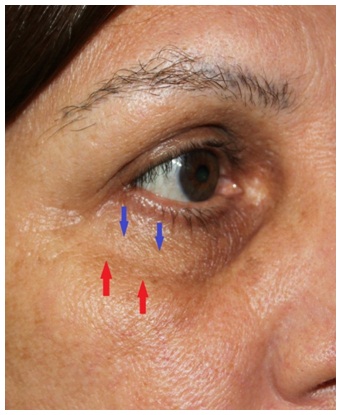
Figure 7: Palpebromalar groove (red arrows), located below the orbital border (blue arrows)
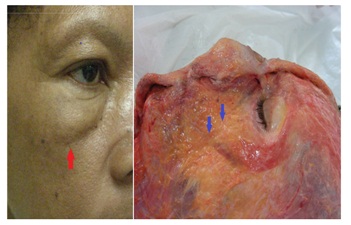
Figure 8: Left: buccal zygomatic groove (red arrow), accentuated by edema. Right: dissection in a fresh cadaver, demonstrating the buccal zygomatic groove showing the limits of the oral cavity and the malar region (blue arrows).

Figure 9: Observe the limits of the oral cavity demarcated by the zygomatic-buccal groove.

Figure 10: V-Shaped deformity, highlighted in red.

Figure 11: Nasolabial groove, formed by the transition of malar excess skin (left) with nasolabial adipose compartment to the labial skin, with scarce subcutaneous and firmly adhered to the orbicularis oris muscle (right), besides the insertions of the superior lip elevator muscles.

Figure 12: Nasolabial groove (blue arrows). Nasolabial subcutaneous adipose compartment (1), and dissected skin over the orbicularis oris muscle evidencing scarce subcutaneous tissue.

Figure 13: Labiomental groove formed by the transition between the excess skin along with the subcutaneous adipose compartment of the jowl, laterally, and the lower labial skin with scarce subcutaneous tissue. The crease may start in the corner of the mouth (left - red arrows), or can be continuous with the nasolabial groove, lateral to the modiolus (right - yellow arrows).

Figure 14: Labiomental groove demonstrated in a fresh cadaver dissection. It is formed by the transition of the cheek skin with the subcutaneous adipose compartment of the jowl to the labial skin, firmly adhered to the orbicularis oris muscle and with scarce subcutaneous. The insertion of the depressor anguli oris muscle also contributes to its formation

Figure 15: Preoperative (left) and one year postoperative (right) a facelift with SMAS plication, frontotemporal elevation, blepharoplasty, and facial lipoplasty
Chat with us on WhatsApp