Citation: Atzori L, et al. Drug Induced Onycholysis. Clin Dermatol J 2017, 2(2): 000114.
*Corresponding author: Dr. Laura ATZORI, Clinica Dermatologica, Via Ospedale 54 09124 Cagliari, Italy, Fax: +390706092580, Tel+390706092324; Email: atzoril@unica.it
Drug-induced onycholysis is a rare, unpredictable, but severe event, whose pain and discomfort is hardly affordable, impairing manual activities or ambulation. Patient’s quality of life might be severely compromised, and correct patient information is mandatory before starting any therapy potentially able to cause it. The course is favorable, with spontaneous remission with drug withdrawal, but complete recovery might take several months due to the slow nail growth rate. Aim of this review is to arouse medical attention on this peculiar type of drug adverse reaction, listing current medications reported as more or less frequent culprit, to recognize the challenge and manage it properly. Patient awareness is critical to prevent and immediately counter act the changes, as well as avoid possible favoring factors, such as contact irritants, trauma, and moisture. Another important issue is recognizing and reporting new observations, as the constant introduction of new drugs will definitely increase the list of possible offending medications.
Keywords: Drug-induced onycholysis; Chemotherapeutic agents; Nail toxicity; Onycholysis; photo-onycholysis
Nail toxicity is a not frequently reported adverse effect of drug administration, although a significant number of classes are implicated, from chemotherapeutic agents [1,2] to retinoids [3], anticonvulsants [4] and immune suppressants [5], including new biologics, such as tumor necrosis factor alpha (anti TNF-alpha) inhibitors [6,7] (Table 1). Reason for relative medical interest may relay on the indolent and prevalent cosmetic valence of several nail changes, especially considering the importance of the treatment for the patient life, but although rarely and unpredictable, onycholysis occurrence is a severe event, whose pain and discomfort is hardly affordable, impairing manual activities or ambulation, with extreme sensitivity to pressure [8]. Patient’s quality of life is severely compromised, and correct patient information is mandatory before starting a therapy potentially able to cause it. The course is favorable, with spontaneous remission with drug withdrawal, but complete recovery might take several months due to the slow nail growth rate. Sometimes the reaction occurs after drug dismissing, because of active principle persistence in the nail plate for longer time than blood half-life. Aim of this review is to arouse medical attention on this peculiar type of drug adverse reaction, listing current medications reported as more or less frequent culprit, to recognize the challenge and manage it properly. Patient awareness is critical to prevent and immediately counteract the changes, as well as avoid possible favoring factors, such as contact irritants, trauma, and moisture. Another important issue is recognizing and reporting new observations, as the constant introduction of new drugs will definitely increase the list of possible offending medications.
Search Strategy and Selection CriteriaA search of MEDLINE and EMBASE databases (1974- 2016) was performed using the terms and variation of terms “onycholysis”, and “drug” or “anticancer”, “immunosuppressive drug”, “photoonycholysis” and “drug” or “antibiotics” , “psoralen”, “aminolevulinic acid”. The retrieved literature was selected to include all relevant articles for appropriate description of drug causality assessment, clinical presentation, diagnosis, incidence, management and treatment of iatrogenous onycholysis and photo-onycholysis.
Clinical PresentationDrug-induced onycholysis is the result of an acute toxic effect on the nail bed epithelium with epidermolysis and loss of adhesion, starting at the distal free margin, causing the detachment of the nail plate from the bed and lateral supporting structures (Figure 1). The newly empty space usually appears white, because of the air interposition, and tends to progress proximally. Formation of hemorrhagic splinters and sometimes blisters is also possible [8]. Less often, separation of the nail plate begins at the proximal nail and extends to the free edge, causing an onychomadesis (Figure 2).The reaction usually affects several nails, mainly of the hands, with symmetrical distribution, but also the feet might be involved (Figure 3), and sometimes all 20 nails are involved [1-8].
An additional event is the interaction with ultraviolet radiation for photosensitive chemical agents, resulting in a photo-onycholysis [9]. The nail plate is completely transparent to the light, without natural sunscreen, and may even concentrate the solar radiation acting as a lens, thus reaching the photosensitizers in the nail bed. By chance, this kind of reaction is quite uncommon in respect to the list of drugs potentially able to induced it (Table 2), including out-of-the counter non-steroidal antiinflammatories. Photo-onycholysis is rare in dark-skinned individuals [8]. Agents most often associated with photoonycholysis usually cause also systemic photo toxicity, but nails changes can occur after a longer time-lapse and sometimes when the drug has been dismissed, because of the different concentration and persistence of the drug in the nail bad and plate. It usually regresses after discontinuation of the causative agent. Clinical presentation is super imposable to conventional onycholysis, although severe pain and hemorrhagic blisters are more frequent, and thumbs are often spared (Figure 4), probably because of their less directly exposed positioning.Three patterns of photo-onycholysis are described [8] although in our experience, same patient presents with a variable mixture of these findings:
Type I: Involvement of several digits, with a distal halfmoon shaped detachment surrounded by a welldemarcated pigmented zone.
Type II: Only one digit is involved and present as a proximal circular notch.
Type III: Several digits are involved, but changes are located in the central part of the nail bed, usually associated with subungual hemorrhages.
Pathogenesis and Implicated DrugsMechanisms of direct nail toxicity are not completely elucidated, but administration schedule is implicated for several drugs, such as antineoplastic drugs and antibiotics, with dose and treatment duration related effects. List of reported drugs (Table 1, 2) and supposed pathogenesis for single categories is extracted from literature retrieval.
Chemotherapeutic AgentsOnycholysis occurs during administration of several anticancer drugs, with characteristic dose-related toxicity, after several weeks of treatment because of the slow nail plate-growing rate [1].
Taxanes: these cytotoxic agents include docetaxel and paclitaxel, which are the most frequent cause of iatrogenous onycholysis, with an incidence ranging from 0 to 44% [10,11]. Docetaxel, more frequently than paclitaxel, induce hemorrhagic onycholysis and subungual abscesses [2,8,12].Several mechanisms might be implicated in taxanes induced nail toxicity, such as the intrinsic antiangiogenic activity and vascular abnormalities, as well as the thrombocytopenia and neutropenic effects from the sympathetic fibers release of neuropeptides and prostaglandins, as well as a direct cytotoxic effect on the nail bed, [2,8-11].
Epidermal growth factor receptor (EGFR) inhibitors: This class of targeted anticancer treatments has a characteristically high dermatological toxicity, which is associated with the rate of clinical response, thus to be considered well-known side effects, and not the adverse events, including acneiform eruption, xerosis, pruritus and nail changes [12-14]. Among these last, nail fold paronychia and pyogenic granuloma-like lesions are the most frequent and debilitating manifestations, while onycholysis is quite uncommon [2,12]. A long term treatment is necessary to induce the toxicity, with 44% of patients manifesting distal onycholysis when receiving any EGFR inhibitor for more than 6 months [14]. Erlotinib (Tarceva) is the representative active principle of the class, with diffuse, bilateral involvement, but also unilateral onycholysis in patient treated for non-small cell lung cancer [15]. Mechanism of action is related to the inhibition of EGFR mediated signaling pathway, with impaired growth and migration of keratinocytes, increased cell attachment and differentiation, increased inflammatory chemokine expression and subsequent cutaneous injury [15].
Specific Protein Kinase inhibitors: Given the role of the mechanistic target of rapamycin (mTOR) and the mitogen-activated protein kinase enzymes (MEK) signaling downstream of EGFR, the pathogenic mechanism of nail toxicity is similar to the EGFR inhibitors class [2]. Duration of treatment is critical to the probability of developing onycholysis, with 50% of patients affected when treated with mTOR for renal carcinoma over a period of 18 months [16]. Two cases of patients who developed a 20 nails dystrophy with fragility and distal onycholysis after 6 months of therapy with temsirolimus are described [17]. Among MEK inhibitor, onycholysis is the most common nail change described during therapy with dabrafenib for metastatic melanoma in BRAF (V600) mutated patients, alone or in combination with other drugs [18].
Antimetabolites chemotherapy: Several studies have linked capecitabine to the development of onycholysis [19], either alone or in combination with other anticancer drugs, such as docetaxel in advanced gastric cancer [20] or irinotecanfor colorectal cancer [21]. The time-lapse before onycholysis occurrence is usually shorter with antimetabolites than targeted therapy, of few months as with high dose methotrexate and leucovorin calcium [1] or in apatient treated with permetrexed for non-small cell lung cancer [22].
Other anticancer drugs: Mitozantrone for metastatic prostate cancer is reported to cause onycholysis, alone or in combination with methotrexate [1,23,24]. Bleomycin and doxorubicin were among the first reported causes of extensive onycholysis, and toxicity is confirmed in more recent scientific literature [8,25,26]. Etoposide, alone or in combination with other cytotoxic agents, was responsible for onycholysis of the finger and toenails [25,27].
Immunosuppressive DrugsLong-term treatment with sirolimus inrenal transplant recipients caused nail alterations, including onycholysis in 42% of cases after a mean duration of treatment of 18 months, with one case of photo-onycholysis [5].
Tumor Necrosis Factor- alpha Inhibitors (anti-TNF alpha): onycholysis is reported as a mild adverse event in 1.8% of rheumatoid arthritis patients treated with any anti-TNF alpha (infliximab, adalimumab,etanercept) for 5 years [7]. Besides, a severe all digits onycholysis has been reported in a HIV positive man during infliximab therapy for Reiter’s syndrome [6,7].
AnticonvulsantOnycholysis is reported in the treatment of epilepsy, especially with valproic acid [28-31] and carbamazepine [32], while hydantoin and trimethadione are listed in a previous comprehensive review [4]. Patient is characteristically young, and the manual activity impairment has a strong impact on their quality of life. The possible mechanism of onycholysis hypothesized for valproic acid is a defective zinc metabolism, caused by a combination of valproic acid–induced deficiency and systemic chelation of zinc [29,33].
RetinoidsThe accelerated desquamation of the stratum corneum in the nail bed is the possible explanation of the rare occurrence of onycholysis, mainly during long-term treatment with isotretinoin [3,8,34].
Additional Drugs Implicated in PhotoOnycholysisThe most obvious cause of photo-onycholysis is as consequence of long-term administration of photosentizing agents during phototherapy, such as psoralen exposure [35,36]. A peculiar report regard a 25- year old male with an extensive vitiligo treated with oral xanthotoxin (ammoidine) on alternate days followed by sun exposure, with marked improvement, but developing a very painful finger and toenails onycholysis after 6 months of therapy [37]. A recently reported source of photo-onycholysis is photodynamic therapy, in patients treated with Aminolevulinic acid and light exposure for actinic keratoses of the hands [38] and face [39].
More unpredictable is the occurrence during antibiotics administration, although the photosensitizing effect of tetracyclines has been widely documented, is dose dependent and mainly due to a phototoxic mechanism [40,41], combined with a cutaneous rash or photoonycholysis being the only finding [42]. Doxycycline is the most frequently cited among this class of antibiotics [42,43]. A severe pediatric case, with hemorrhages of the proximal nail folds, developed after a week therapy for periodontal disease [44]. The therapy with doxycycline was interrupted and the nails returned normal after 3 months.
Other antibiotics frequently reported to induce photoonycholysis are fluoroquinolones, such as pefloxacine and ofloxacin [45,46].
Another class of widely diffused, out of the counter drugs potentially related to the development of photoonycholysis are the non-steroidal anti-inflammatories, especially benoxaprofen and indomethacin [47-49], but also more recently marked agents, such as diclofenac [50].
Among antifungals, the old but always reference treatment for dermatophyte infections, griseofulvin has been associated with photo-onycholysis [51]. More recently, voriconazole use for a primary cutaneous aspergillosis has been implicated in pseudoporphyria and photo-onycholysis development in a pediatric patientwith acute lymphoblastic leukemia [52].
Several old neuroleptic agents were abandoned for the risk of photo toxicity, nevertheless one of the new atypical antipsychotic indicated for the bipolar disorder, olanzapine has been recently implicated in a case of photo-onycholysis after 1 month of treatment, who substitution with aripiprazole causes a worsening, both in the number of nails and surface affected [53].
Oral contraceptives have been implicated in anecdotal cases of photosensitivity, but recently a well-documented case of finger photo-onycholysis and porphyria cutaneatarda in 21-year-old woman has been described [54].
DiagnosisOnycholysis is a clinical diagnosis, but drug causality assessment might be a challenging process, because symptoms might occur several weeks to months after the drug introduction, sometimes after dismissing the drug, because of the peculiar slow nail rate of growth, taking about 40 days to grow from the proximal nail fold [55]. Any medication taken in the past 2–3 weeks before the onset of the nail symptoms should be suspected [1]. When nails changes occur in the context of a generalized drug adverse reaction (Figure 5), the diagnosis is obvious, but sometimes onycholysis is the only manifestation. In this case, the iatrogenous causality assessment follows the rules of any adverse event [56]: accurate clinical history, temporal relation with drug intake, exclusion of alternative etiologies, and improvement with drug withdrawal (de-challenge). An additional criteria, not obligate because exposing the patient to a more severe reaction, is worsening with drug repeated administration (re-challenge). Sometimes this information comes from clinical history, especially for pulse treatments, such as chemotherapy [1].
Differential diagnosis include toxicity in the setting of a general systemic reaction, such as graft-versus-host disease, with often severe onycholysis not actually related to the high dose chemotherapy, but to the bone marrow transplantation itself [1]. Besides, the oncologic neutropenic state and general immunosuppression are risk factors for secondary nails infection, which remain the main condition to be excluded. Thus, repeated bacteriological samples and mycological examinations are indicated. Onychomycosis is usually sufficiently investigated performing a direct potassium hydroxide wet mount, but fungal cultures is sometimes indicated to evaluate the cure rate after antifungal therapy and/or identification of responsible species [57]. Nail biopsy and histological examination is very rarely performed, being a painful invasive procedure, with a high risk of not specific findings, but sometimes necessary to exclude major nails pathologies, including lichen planus or psoriasis, not necessarily drug-related. Staining of the specimen with periodic acid – Schiff (PAS) is indicated to further exclude the presence of hyphae in the stratum corneum in onychomycosis.
TreatmentSymptoms are reversible, but a certain discomfort might persist until the nail plate grows completely tight to the nail bed. Patients should keep nails short, clipping detached portions every 1-2 week (Figure 6), and maintain the nail bed dry after each hand washing with antiseptic solutions, such as chlorhexidine or local antibiotic, such as mupirocin. Prevention of microbial colonization is mandatory especially in patients under chemotherapy and severely immunosuppressed, and in all cases with sub-ungueal hemorrhages and bullae [58].Another important measure is wearing light cotton gloves under vinyl gloves for wet work.
With drugs potentially able to cause photo-onycholysis, additional measures are avoidance of excessive sunexposure and application of colored nail polish to protect thenail bed [59].
Docetaxel-induced onycholysis may be prevented by wearing a frozen glove for 90 minutes during infusion of the chemotherapeutic agent [60,61].
In case of severe and painful onycholysis, it may be useful to sting under the nail plate and release the accumulated fluids, more rarely it is necessary to remove the nail plate [10].
ConclusionOnycholysis is a very characteristic adverse effect of drugs administration, which can affect patient’s daily activities and quality of life, thus requiring correct information prior the initiation of any treatment potentially able to cause it. Several life-saving drugs are implicated, such as traditional and targeted chemotherapies, although incidence is variable and probably underestimated. Pathogenesis is not completely clear, but is the result of a direct toxic effect on the nail, which is unpredictable, but dose and time dependent, with variable time-lapse depending on the causative agent. The role of the dermatologist is crucial to explain the possible implications, but also reassuring on the transitory of the changes, suggesting adequate preventive measures, as well as prescribing curative strategies to adopt at first signs of onycholysis occurrence. Correct information prevents excessive anxiety, and discomfort especially in woman under chemotherapy, considering the impact of nails and hairs changes on self-esteem and femininity, so heavily affected by the cancer itself. Patient’s lifestyle and profession should also be considered to avoid unplanned contingency.

Figure 1: Taxane-induced onycholysis in a 45-year-old man causing half nail white detachment, and splinters hemorrhages of several fingers, including the thumbs. Some nails of the right hand were affected in a previous episode, and the distal portion clipped short already.

Figure 2: Proximal extension of the onycholysis in a taxane exposed woman

Figure 3: Involvement of the feet in the same patients, with painful subungual hemorrhages and distal onycholysis of the big toes.

Figure 4: Photo-onycholysis during psoralen phototherapy: sparing of the thumbs, half-moon shaped detachment of some digits, proximal pigmentation and circular notch of the 3rd digit of the left hand, subungueal hemorrhages with complete central part of the nail bed of the 2nd and 3rd finger of the right hand. Variable severity probably depends on hands positioning during UV exposure.

Figure 5: Severe onycholysis of the feet in a patient with Toxic Epidermal Necrolysis.

Figure 6: Onycholysis recovery, with detached portions regularly clipped until complete adhesion of the nail plate to the nail bed.
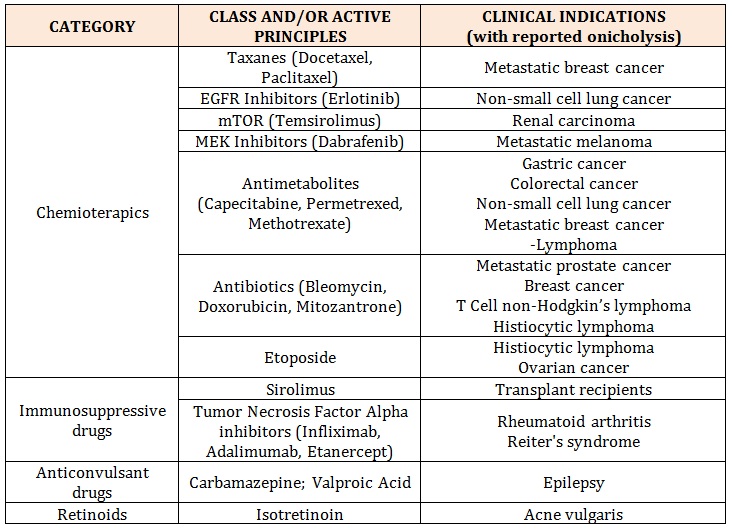
Table 1: List of the drugs reported to induce onycholysis.
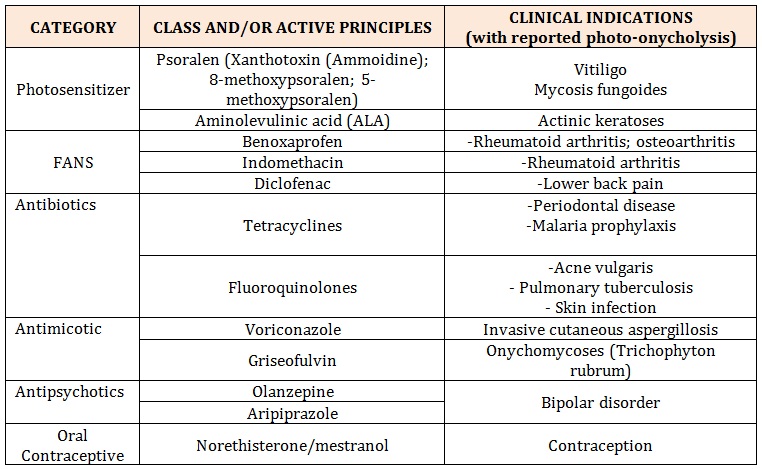
Table 2: List of the drugs reported to induce photo- onycholysis.
Chat with us on WhatsApp