Citation: Albugeaey M, et al. Superiority of Split-Dose Bowel Preparations for Morning and Afternoon Colonoscopies: A Single Center Experience. Gastroenterol Hepatol Int J 2017, 2(2): 000120.
*Corresponding author: Mohammed Albugeaey, MD, Division of Gastroenterology and Hepatology, Medstar Georgetown University Hospital, 3800 Reservoir Rd NW – Main Bldg 2nd floor, Washington, DC 20007, USA, Email: mohammed.a.albugeaey@gunet.georgetown.edu, malbugeaey@hotmail.com
Background: ASGE guidelines recommend SPLIT for afternoon colonoscopies and when feasible for morning procedures. We compared the effects of different bowel preparations given as SPLIT vs. SINGLE on the quality of bowel preparation.
Methods: In a University Hospital, all adult outpatients undergoing colonoscopy were offered the opportunity to participate in this survey during September and October 2015. Patients undergoing both screening and non-screening colonoscopies were included. 611 of 1002 asked patients filled out a survey. The Boston Bowel Preparation Scale (BBPS) was used to rate the preparation. We added a third component that determined how much cleaning effort was required.
Results: SPLIT preparation, using a clear liquid diet and ingestion of 75% or more of the preparation were all associated with a statistically significant quality of bowel preparation and less colon irrigation. The study compared SPLIT vs SINGLE regimens, revealing the superiority of SPLIT dosing regardless of the timing of the colonoscopy, the gender of patients or the type of preparation. Only 3.8% of patients receiving SPLIT dose had a poor preparation compared to 11% of poor preparation with SINGLE. The need for repeat colonoscopy due to poor preparation was 6.2%.
Conclusion: Our study confirms the superiority of SPLIT and clear liquid diet for both morning and afternoon colonoscopies. There was no significant difference in the quality of bowel preparations between different solutions. We recommend SPLIT for all colonoscopies regardless of timing.
Keywords: Colon cancer screening; Screening colonoscopy; SPLIT bowel preparation; Poor bowel preparation; Quality improvement
Colonoscopy is the most effective method to evaluate the colon. It has both diagnostic and therapeutic utility. It can be technically difficult if the colon is not optimally prepared [1]. Standards of this procedure include a completion to caecum rate of 90% [2]. Inadequate bowel preparation is significantly associated with incomplete colonoscopies, and subsequently completion rates below 90% [3,4]. An ideal bowel preparation is one that efficiently discharges bowel contents and is tolerated by patient, without risk of complications. Rates of poor preparations requiring a repeat colonoscopy range between 7% and 25%. The large volume of preparation used (3-4L) and the adherence to clear liquid diet for a full day prior to procedure makes these bowel preparations cumbersome to patients. The three commonly used agents are polyethylene glycolbased electrolyte solution (PEG-ELS), osmotically active agents, and stimulant laxatives. Some regimens combine these agents. The American Society for Gastrointestinal Endoscopy (ASGE) guideline for bowel preparation prior to colonoscopy indicates that giving part of the bowel preparation dose on the same day of colonoscopy (termed SPLIT dose) results in a higher quality colonoscopy examination compared with ingestion of the entire preparation on the day or evening before colonoscopy [5]. SPLIT-dosing also improves patient tolerance and willingness to repeat the procedure using the same preparation [5].
This prospective study compares the effects of different bowel preparations given as SPLIT versus SINGLE-dose, along with other factors, on the quality of bowel preparation prior to colonoscopy and patient tolerability and satisfaction.
Patients and MethodsIn our University Hospital Endoscopy Center, we offered all adult outpatients undergoing colonoscopy the opportunity to participate in this study. Patients undergoing both screening and non-screening colonoscopies were included. Exclusion criteria were the following: presence of active colitis, presence of colonic resection or presence of active gastrointestinal bleeding. We did not collect data of patients who suffer from chronic constipation, uncontrolled diabetes mellitus or on chronic opioids. The study was conducted between September 1st 2015 and October 31st 2015. The number of patients who had a colonoscopy during the study period was 1002. After obtaining informed consent, 611 patients (61%) agreed to fill out a survey regarding their gender, the type of preparation solution, how it was taken (SPLIT vs SINGLE), the volume ingested, whether they adhere to a clear liquid diet the day prior to colonoscopy, the time to first bowel movement, morning versus afternoon procedure and whether this was a first time versus subsequent colonoscopy. All patients underwent continuous monitoring of blood pressure, heart rate, respiratory rate and oxygen saturation during the procedure and recovery period. All cases were done under monitored anesthesia care (MAC). The study protocol was reviewed and approved by the institutional review board of our University.
Bowel Preparation InformationBowel preparations were prescribed according to gastroenterologist and patient preference. The four types of preparations used were Colyte® (Polyethylene glycol electrolyte solution PEG-ELS, volume= 4L), Miralax® (PEG-3350-SD, volume= 238 grams in 2L), Prepopik® (sodium picosulfate/magnesium oxide/anhydrous citric acid, volume= 10 oz plus 2L of liquid), and Moviprep® (low-volume PEG-ELS with ascorbic acid, volume= 2L of preparation plus 1L of liquid). Additives such as magnesium citrate or bisacodyl were allowed. All patients were instructed to avoid nuts, seeds, corn and popcorn for seven days prior to their colonoscopy. All patients were allowed to consume jello, clear broth and clear juices. The dosing type of the preparation (SPLIT versus SINGLE) was assigned to patients ahead of time. SINGLE-dose bowel preparation was defined as consuming all the liquid at once the day before the procedure, between 5pm and 8pm. SPLIT-dose bowel preparation was defined as consuming the first half of the prescribed volume the day prior to colonoscopy, between 5pm and 8pm, and the second half ingested at a minimum of six hours before the scheduled colonoscopy. All patients had access to call an on-call gastroenterology fellow or mid-level provider for any questions or concerns regarding their bowel preparation.
Data Collection from PatientsThe day of colonoscopy, patients were asked to fill out a questionnaire composed of eighteen questions prior to the procedure (see appendix). The questions evaluated the type of bowel preparation the patient ingested, dosing type (SPLIT or SINGLE), the volume consumed (as 100%, 75%, 50% or <=25%), the type of diet patient had the day prior to procedure (clear liquid or solid food),the time to a first bowel movement , the timing of colonoscopy (morning or afternoon), whether this was their first colonoscopy or subsequent procedure, the occurrence of any adverse events (abdominal pain, nausea, vomiting, bad taste or other), the clarity of instructions provided by the gastroenterology department , the payment method for the preparation, a patient satisfaction on a scale from 1 to 5, and their willingness to retake the same bowel preparation in the future and whether they would recommendthis bowel preparation to family or friends for their procedures.
Bowel Cleansing AssessmentGastroenterologists performing the colonoscopy were asked to fill out a survey at the end of the procedure which evaluated the quality of bowel preparation before and after cleaning efforts. The amount of time spent cleaning was documented as minimal or no cleaning, moderate or extensive effort which was entirely subjective to the gastroenterologist judgement. The postprocedure survey also included the need for a repeat colonoscopy due to poor preparation, detection of polyps, detection of diverticular disease and any other comments regarding bowel preparation. The Boston Bowel Preparation Scale (BBPS) was used to rate the quality of the preparation using both pre and post-cleaning scores (figure 1). BBPS was developed in Boston University Medical Center and published in 2009 [6]. It utilizes is a four-point scoring system applied to each of the three broad regions of the colon: the right colon (including the cecum and ascending colon), the transverse colon (including the hepatic and splenic flexures) and the left colon (including descending colon, sigmoid colon and rectum). The points are assigned from 0 to 3 as follows: 0=Unprepared colon segment with mucosa not seen due to solid stool that cannot be cleared; 1=Portion of mucosa of the colon segment seen, but other areas of the colon segment not well seen due to staining, residual stool and/or opaque liquid; 2=Minor amount of residual staining, small fragments of stool and/or opaque liquid, but mucosa of colon segment well seen; 3=Entire mucosa of colon segment seen well with no residual staining, small fragments of stool or opaque liquid [6]. Each region of the colon receives a score from 0 to 3 [6]. Total BPPS scores range from 0 to 9, with 9 reflecting a perfectly clean colon without any residual liquid and 0 reflecting an unprepared colon [6]. As it is currently used, the BBPS evaluates bowel preparation quality after all cleaning efforts have been applied. Scores for this study, we included both pre- and post-cleaning scales. All full-time faculty gastroenterologists who participated in this study were trained on using the BBPS to reduce inter-individual variability.
Statistical Analysis ResultsFifty-three patients were excluded either due to exclusion criteria or incomplete forms; subsequently, our study population included a total of 558 patients.Most patients received Colyte® or Miralax® with Gatorade®. Fewer patients received Prepopik®. Other preparations were given in numbers too small to compare.Amongst the variables taken into consideration, results showed that dosing type (SPLIT versus SINGLE-dose), volume of preparation consumed and type of diet the day prior to colonoscopy (clear liquid versus solid) significantly affect the quality of bowel preparation (evaluated with BBPS score) and the amount of cleaning required by endoscopist during procedure (Table 1). BBPS average score difference was statistically significant with SPLITdose preparation compared to SINGLE-dose, both before (pre) and after (post) cleaning (p-value=<0.0001). Average scores with SPLIT preparation were 7.8 and 8.5 respectively pre and post cleaning, whereas with SINGLE preparation scores were 6.8 and 7.8 for pre and post cleaning respectively. Furthermore, consumption of 75% of the preparation or more was significantly associated with better BBPS average score (p-value=0.0039 for precleaning; p-value=0.0006 for post- cleaning). In addition, clear liquid diet was significantly linked to a higher BBPS average score compared with solid diet the day prior to colonoscopy (p-value=0.0039 for pre-cleaning; pvalue=0.0006 for post- cleaning). With regard to amount of cleaning performed by the endoscopist to better visualize the colon, our results revealed three statistically significant findings. First, SPLIT preparation lead to a lower amount of moderate and extensive cleaning compared to SINGLE-dose preparation (pvalue=<0.0001). Although, the procedure time was not measured, minimal cleaning hypothetically should shorten the procedure time. Second, consumption of 75% or more of bowel preparation resulted in a decreased amount of patients requiring an extensive amount of cleaning when compared to a volume consumption less than 75% (p-value=<0.0001). Third, adherence to a clear liquid diet the day before colonoscopy was associated with a reduced need for a moderate and extensive cleaning when compared to solid diet (pvalue=<0.0001).The type of preparation solution, time to first bowel movement, timing of colonoscopy whether in the morning or afternoon and first versus subsequent colonoscopy were all variables that did not significantly affect the outcome (Table 1). There was no statistical difference in BPPS between males and females.
Results were adjusted to compare SPLIT and SINGLEdose preparations using the following variables: type of preparation solution, type of diet, gender, timing of colonoscopy, time to first bowel movement and presence of diverticulosis. We based the comparison on average BBPS scores pre-cleaning only. The results showed statistically significant superiority of SPLIT regimen in both males and females who received Colyte or Miralax, and had clear liquid diet the day before colonoscopy, regardless of timing of colonoscopy or time to first bowel movement. As a matter of fact, patients who ingested Colyte or Miralax had higher score when they split the preparation (p-value<0.0001 and p-value=0.0003, respectively) whereas ingestion of Prepopik® or other preparation did not show statistically significant difference probably because of small numbers. Patients who had a SPLIT preparation and clear liquid diet had average BBPS of 7.89, which is higher than average BBPS of 6.87 in patients who had SINGLE-dose preparation and clear liquid diet (p-value<0.0001). SPLIT versus SINGLEdose preparation did not show statistically significant effect on BBPS scores in patients who had non-clear liquid diets (p-value=0.2527). SPLIT-dose preparations were equally superior in both males and females (pvalue<0.0001 in both groups), and similarly in morning and afternoon procedures (p-value<0.0001 in both groups) (Table 2). The presence of diverticulosis did not significantly affect the scoring (p-value=0.7138).
Finally, the need for repeat colonoscopy due to poor preparation was 6.2% in our patient population which is lower than the national average rate (16.9%-23.1%) [7- 9].
DiscussionThe ASGE recommends SPLIT-dose regimens for all patients and/or same day preparations for afternoon colonoscopies with a portion of the preparation taken within 3 to 8 hours of the procedure to enhance colonic cleansing and patient tolerance [5]. Studies show that approximately 1 in 4 to 1 in 6 patients have inadequate bowel preparation for colonoscopy [7-9]. Adenoma miss rates as a consequence of suboptimal bowel preparations are high. Lebhowl et al. conducted a study on 216 patients who had colonoscopies done with suboptimal bowel preparation followed by a complete colonoscopy with optimal bowel preparation, and concluded that overall adenoma miss rate among these patients was 42% for all adenomas and 27% for advanced adenomas [7]. Chokshi et al. reported 34% missed adenomas among average risk patients undergoing repeat colonoscopies [10]. Missed adenomas can potentially develop into cancer, and have unwanted consequences on patients. When bowel preparation quality is compromised, some gastroenterologists advise a prompt repeat of colonoscopy, while others advocate in favor of shortening the interval for subsequent colonoscopy [11,12]. The need to repeat colonoscopy comes with its own obvious disadvantages, including increased cost and inconvenience to patients.
In our study, we found that SPLIT bowel preparations, clear liquid diet the day before colonoscopy and consuming at least 75% of the preparation volume are statistically significant variables that improve the quality of bowel preparation for both morning and afternoon colonoscopies. In addition, the amount of cleaning required by gastroenterologists during the procedure was significantly less with SPLIT preparation. These findings were accompanied by statistically significant superiority of SPLIT compared to whole dose preparation when the patients received Colyte or Miralax and clear liquid diet regardless of their gender, timing of colonoscopy and presence or absence of diverticulosis. Additionally, the present study showed a need for repeat colonoscopy of 6.2%, which is lower than the national average rate.
Our study provides data that are in agreement with other studies in the literature comparing SPLIT vs SINGLE. For instance, Church et al. found that giving patients undergoing afternoon colonoscopies the preparation on the same day resulted in significantly better cleansing in all areas of the colon [13]. Moreover, El Sayed et al. showed that bowel preparation with SPLITdose PEG-electrolyte solution results in a significantly greater quality of colon cleansing, with better compliance and no additional adverse effects or discomfort to the patients [14].
Interestingly, recent studies are emerging, suggesting that the use of low-residue diet the day before colonoscopy improves tolerability by patients and willingness to repeat preparation, with no differences in preparation quality and adverse effects [15].
This study has some limitations which must be pointed out. First, we did not collect data about patients’ comorbidities which could affect the results, such as chronic constipation, diabetes mellitus and chronic opioids use. Second, the study was not blinded. The gastroenterologist was aware of type of the bowel preparation consumed prior to performing the procedure. However, the patients were unaware they were going to participate in the study until the day of the procedure. Third, we had a very small number of patients who used Moivprep®.
ConclusionOur study confirms the superiority of SPLIT preparation and clear liquid diet not only for afternoon colonoscopies but for morning procedures as well. There was no significant difference in the quality of bowel preparations between different preparation solutions. We believe that SPLIT regimen could ultimately reduce unnecessary costs by preventing repeat colonoscopy due to poor preparation quality. Further studies are required to assess the non-inferiority of low-residue diets compared to clear liquid diet in regard to bowel preparation quality, since less dietary restrictions have been associated with higher patient satisfaction and willingness to repeat preparation.
DisclosureThe authors have no financial disclosures to declare. Authors have no actual or potential conflict of interest in relation to this project. The Division of Gastroenterology & Hepatology at Medstar Georgetown Univeristy Hospital does not endorse any of the bowel preparations listed in this project.
AcknowledgementSpecial thanks to Sameer Desale for statistical analysis. Biostatistics and Bioinformatics, Medstar Health Research Institute, Hyattsville, MD. Stephanie Yan, medical student, for assistance in data collection. Georgetown University School of Medicine. Avantika Mishra, internal medicine resident for assistance in data collection. Medstar Georgetown University Hospital.
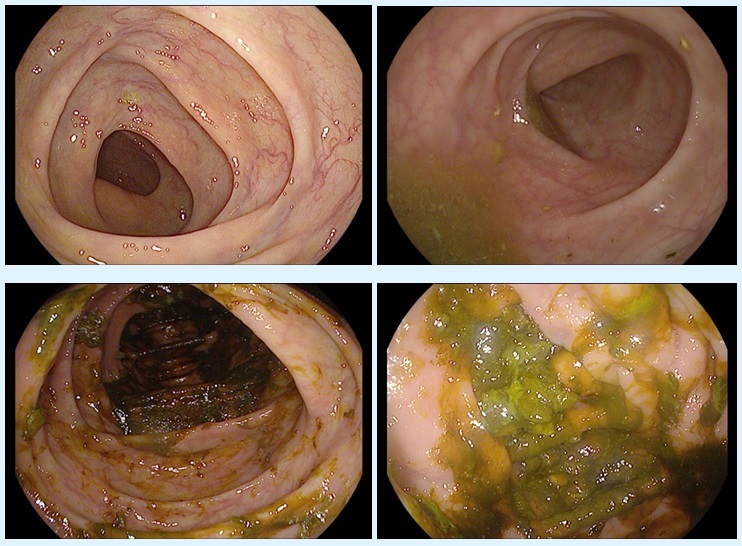
Figure 1: The Boston Bowel Preparation Scale (BBPS). BBPS 3 (A), BBPS 2 (B), BBPS 1 (C) and BBPS 0 (D).
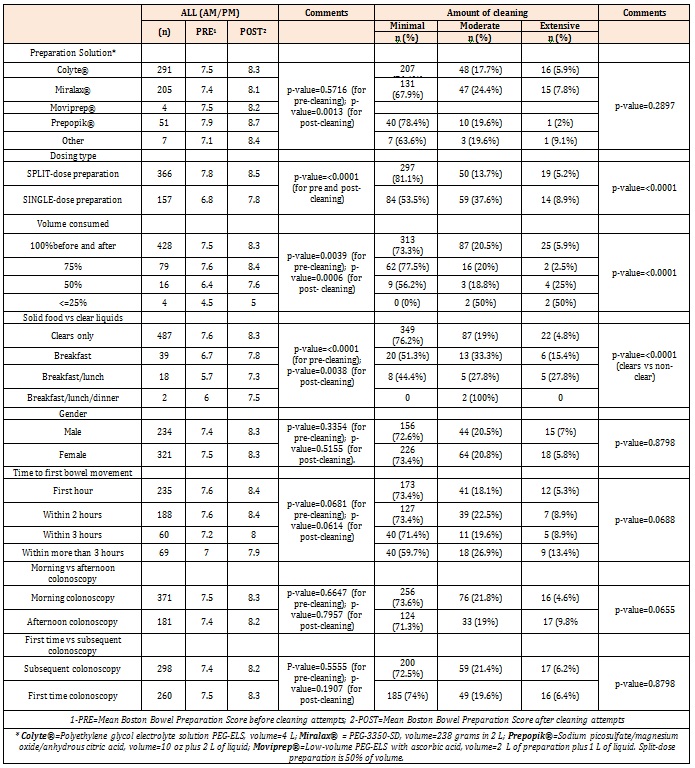
Table 1: Results comparing pre and post cleaning Boston Bowel Preparation Score and amount of cleaning.
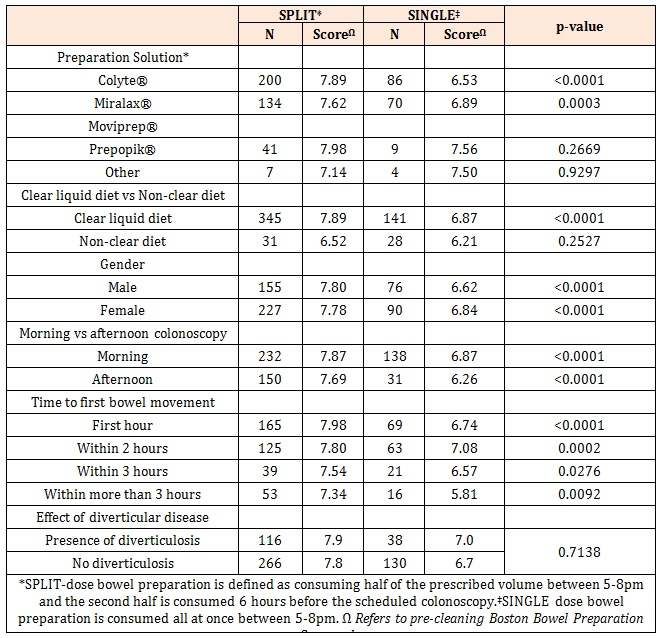
Table 2: Results adjusted comparing SPLIT and SINGLE bowel preparation.
Chat with us on WhatsApp