Citation: Arnelo U. Continuous Intrabiliary Acetylcysteine Infusion Allowed Perioperative Chemotherapy in a Jaundiced Patient with Malignantly Transformed IPMN and Pancreatobiliary Fistula. Gastroenterol Hepatol Int J 2017, 2(2): 000124.
*Corresponding author: Urban Arnelo, Karolinska University Hospital Huddinge, K53, 14186 Stockholm, Tel: 004964215866460, Email: alexanderwaldthaler@gmail.com
We report the case of a patient with a malignantly transformed IPMN (intraductal papillary mucinous neoplasm) of the pancreatic head with involvement of the common bile duct (CBD) and borderline resectability. Due to jaundice, immediate cytostatic treatment was not possible. The patient underwent several ERCPs (endoscopic retrograde cholangiopancreatography) with implantation of plastic and metal stents. However, resolution of jaundice could not be achieved. Therefore, a therapy with acetylcysteine was initiated, first orally, then with intermittent and finally continuous biliary flushing, which led to normalization of bilirubin levels. Intraductal biliary treatment with acetylcysteine has previously been described, but only in a palliative setting. This case shows that continuous percutaneous infusion of acetylcysteine into the biliary tree can contribute to the therapy of cholestasisin selected patients with IPMN and borderline resectability by resolving mucus occlusions and thereby allowing a curative approach with perioperative cytostatic treatment.
Keywords: Acetylcysteine; Borderline; Continuous flushing; ERCP; Fish mouth; IPMN; Jaundice; mucus; Pancreatobiliary fistula; Pig nose
IPMN is a cystic tumor of the pancreas associated with the production of mucus. Usually the mucus produced by the tumor is clear and thick leading to characteristic clinical features such as the so called fish eye papilla or fish mouth papilla. A rare complication of IPMN is formation of pancreatobiliary fistula. Here, mucus from the IPMN reaches and obstructs the common bile duct (CBD) which may cause the major duodenal papilla to take the shape of a pig nose. Stenting is of limited benefit and the prognosis for patients with this manifestation has been poor if surgery cannot be performed as single therapy [1]. The effects of acetylcysteine on the production of mucus are described in several organ systems and experimental work has been done on the potential effects in gastrointestinal tumor therapy [2]. So far, intraductal biliary treatment with acetylcysteine has previously been tried only in a palliative setting [3,4]. Perioperative chemotherapy is gaining significance in pancreatic malignancies with borderline resectability. Jaundice is a common complicating factor that can be resolved by internal drainage via ERCP in most cases. In some patients with tumors producing tough mucus, the sole establishment of an outflow is not sufficient. A therapeutic approach using acetylcysteine seems promising. Exceeding its mucolytic activities, acetylcysteine has antioxidant and anti-inflammatory properties. Except for allergic predispositions, to our knowledge, there are no contraindications for the use of acetylcysteine.
Case ReportWe hereby report a case of a 46 year old male patient who was diagnosed with IPMN of the pancreatic head with involvement of the CBD and borderline resectability. EUS guided needle biopsy supported the diagnosis of a malignantly transformed IPMN. At the time of diagnosis, no distant metastasis could be detected. However, the tumor was locally advanced with involvement of the superior mesenteric artery (SMA) and vein (SMV) (figure1). Clinically the patient presented with dyspepsia, weight loss, right upper quadrant pain and jaundice. A preoperative down staging cytostatic treatment was recommended by an interdisciplinary board prior to surgery. However, immediate cytostatic treatment was not possible due to jaundice. An ERCP was performed which showed an enlarged papilla with clear mucus in the orifice. The typical pig nose appearance was exposed after saline clearance (figure 2a and 2b) [5]. During the first ERCP two plastic stents were placed in the CBD. A second ERCP was performed and five new plastic stents were introduced. None of these procedures led to a significant and persistent improvement of symptoms or to a resolution of jaundice. During the third ERCP the CBD was 20 mm wide and thick, almost solid pieces of clear mucus obstructed the outflow. Even though a 15 mm balloon could be easily pulled through the papilla, the chunks of mucus could not be extracted mechanically. The papilla was dilated to 20 mm and two fully covered 10 x100 mm self-expandable metal stents (SEMS) [BSc Wall flex] were placed side by side in the common bile duct. Oral administration of acetylcysteine (400 mg x 5 per day) was initiated one day after the procedure. These treatments controlled the biliary stasisonly temporarily. Two weeks later, during a fourth ERCP, the SEMS needed to be cleared from mucus again and a nasobiliary catheter was placed for intermittent acetylcysteine infusion (300mg x3 per day). Since this did not improve the jaundice sufficiently enough to allow a cytostatic treatment and the patient developed cholangitis, the nasobiliary catheter was removed and replaced by a percutaneous transhepatic catheter (PTC), ending in the common hepatic duct just above the SEMS (fig 3). The SEMS were cleared by ERCP and the biliary tract was continuously flushed with acetylcysteine solution (8 000mg ACC in 1000ml saline solution/24h) through the PTC. We observed immediate decline in the bilirubin level and our patient reported clinical improvement of symptoms under this treatment. Thus our patient could be discharged from the hospital. He carried the solution in a backpack allowing him to resume his daily activities. Twelve days after the continuous acetylcysteine infusion was initiated, the SEMS needed to be cleared via ERCP for the last time. The bilirubin level was normalized and chemotherapy could be administered. 60 days after the start of the continuous infusion of acetylcysteine via PTC, the bilirubin level was still normal and a pylorus preserving resection of the pancreatic head was successfully performed. The intraoperative frozen section analysis showed no tumor involvement of the resection margins. However, the final histopathological examination showed tumor cells on the resection border to the SMA, regional lymph node metastasis (7/52) and perineural tumor infiltrates. Despite this outcome, this case shows that continuous percutaneous infusion of acetylcysteine in the biliary tree can contribute to therapy of cholestasis by resolving mucus occlusions in selected patients with IPMN and borderline respectability which may allow a curative approach with perioperative cytostatic treatment.
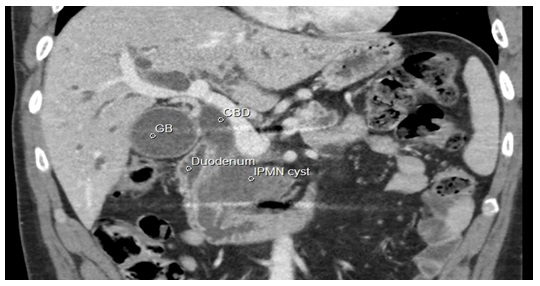
Figure 1: The CT scan shows the IPMN bulging into the wide CBD.
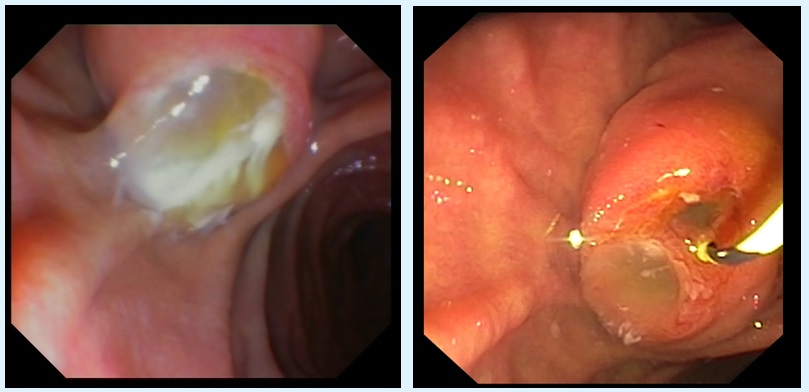
Figure 2: The papilla Vateri in a 46 years old man with IPMN presented with the characteristic fish mouth (figure 2a) appearance. After saline flushing the pig nose (fig 2b) typically seen in patients with pancreatobiliary fistula was revealed.
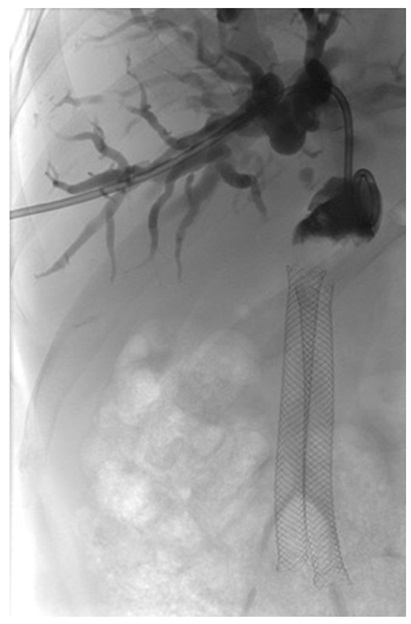
Figure 3: PTC in the common hepatic duct revealing obliteration of the SEMS before clearance and acetylcysteine treatment.
Chat with us on WhatsApp