Citation: Qiang Z, et al. Application and Failure Experience of Intramedullary Nail and Locking Plate in the Treatment of Femoral Subtrochanteric Fracture. J Ortho Bone Disord 2017, 1(1): 000102.
*Corresponding author: Zheng Qiang, The orthopedics department of 2nd affiliated hospital of medical college of Zhejiang university, Zhejiang, China, Tel: 86-15855080807; Email: jljly2339@163.com
Background: The experience of intramedullary nail and locking plate in femoral subtrochanteric fracture were retrospectively analysed.
Methods: The operation time, bleeding, hospitalization, fracture healing time, Harris function score and postoperative complications were summarized between two groups.
Results: The operation time, bleeding, hospitalization, fracture healing time and Harris function score all made no significant differences between two groups. Three cases in nail group and two cases in plate group suffered fixation failure.
Conclusion: Intramedullary nail must focus on fracture reduction and recovery of femoral medial support, whereas locking plate must strictly abide the MIPO technology
Keywords: Femoral subtrochanteric fracture; Intramedullary nail; Locking plate; Internal fixation failure
Femoral subtrochanteric fracture is not uncommon in clinical practice, especially in elderly patients, accounting for 2%−7% of all proximal femoral fractures [1]. This type of fracture remains a challenge to orthopaedic surgeons. Fracture instability and regional muscle traction often render fracture reduction difficult and cause non-union of fracture and failure of internal fixation. According to the mainstream view, fracture fixations can be divided into intramedullary nail and locking plate. However, the type of fixation that is more suitable for treatment remains controversial, and the advantages and disadvantages of each of these approaches remain incompletely understood.
The intramedullary nail treatment is currently the more dominant method used to treat subtrochanteric fractures. Intramedullary nail fixation generally offers more advantages in terms of fixation rigidity, surgical injury, and fracture healing [2]. However, some fracture types, such as long spiral fracture, may not be suitable for intramedullary nail fixation [3]. Although many reports have shown that intramedullary nail have achieved satisfactory clinical effect in treatment of femoral subtrochanteric fracture, there exist some disadvantages in the use of this approach, including long learning curve, increased intraoperative fluoroscopy, failed closed reduction in some fracture types, failure to insert nails in some patients with femoral morphology abnormalities and missing femoral medial support leading to fracture non-union and intramedullary nail failure [1]. The meta analysis of Liu et al. [4] have shown that intramedullary nail fixation offers significant advantages in reducing internal fixation failure, in improving fracture healing and in reducing revision surgery compared with extramedullary fixation. Many clinical reports have shown that the locking plate treatment can also achieve satisfactory clinical efficacy through indirect reduction [5,6]. Li et al. [7] used inverted femoral LISS plate to treat femoral subtrochanteric fracture, and they achieved good clinical results. All patients displayed good bone healing and postoperative hip joint function without serious complications. Kim et al. [8] used prebending femoral compression locking plate and they also achieved excellent results. However, AImerci et al. [9] speculated that inverted LISS prolongs fracture healing, prolongs full weight bearing time and reduces the Harris score of hip joint. Among the current options, the locking plate treatment achieves good clinical results in most instances. However, whether locking plate treatment will increase fracture non-union, fixation failure and revision surgery remains controversial. In addition, whether this treatment will reduce hip joint function remains unclear.
Therefore, the more appropriate choice of fixation choice in subtrochanteric fracture treatment remains disputed. We retrospectively analysed femoral subtrochanteric fracture patients, who were recently treated in our hospital. We attempted to identify the advantages and disadvantages of intramedullary nail and locking plate in the treatment of subtrochanteric fracture by comparing the two groups in terms of clinical data, surgical treatment and clinical results. In particular, we focus on the following aspects: (a) how to restore femoral medical support and avoid the fixation failure in intramedullary nail treatment in some difficult reduction fractures; (b) whether the locking plate will increase fixation failure and fracture non-union incidence; and (c) summary of the failures we experienced in intramedullary nail and locking plate treatment. We hope that this report will serve as a reference for the treatment of femoral subtrochanteric fracture and for selection of internal fixation.
Materials and MethodsThe patients with femoral subtrochanteric fracture and have undergone surgery in our hospital from 2009.1– 2014.12 were retrospectively analysed. The inclusion criteria are as follows: (1) the fracture line is located in the area extending from the lesser trochanter up to 5 cm distal to the lesser trochanter [10]; (2) fracture time relative to the initial operation is < 3 weeks; (3) closed fracture; and (4) follow-up time is longer than 12 months. The exclusion criteria are as follows: (1) open fracture and (2) presence of a pathological fracture or the affected joint had arthritis history. The patients were divided according to internal fixation type. The procedures followed were in accordance with the ethical standards of our hospital committee on human experimentation.
A total of 31 patients were included in the intramedullary nail group, consisting of 22 males and 9 females, and their mean age was 54.8 years old (24–87 years old). The causes of injury in these patients were as follows: tumbles in 21 cases, falls from height in 3 cases, traffic accident in 6 cases, heavy extrusion in 1 case and 6 cases showed combined injuries. A total of 20 patients in the locking plate group were analysed, including 14 males and 6 females, and their mean age was 61.9 years old (27– 82 years old). The cause of injury in these patients were as follows: tumbles in 12 cases, falls from height in 2 cases, traffic accident in 6 cases and 5 cases showed combined injuries.
Treatment methodsThe patients were admitted in our hospital after a definite diagnosis; they received routine preoperative femoral X-ray and femoral CT examination and lower limb traction was continued until surgery. In addition, combined injury, if any, was managed. The Seinsheimer femoral subtrochanteric fracture classification [11] was verified by the preoperative X-ray and CT results. The internal fixation was decided by the doctor, and the combined injury was treated in the same period or in the second stage of operation depending on the patient’s specific circumstances.
Surgical methodsIntramedullary nail: We used long reconstruction nail (Smith & Nephew, USA) or long PFNA nail (Synthese, Switzerland) as fixation. The patients were administered with general anaesthesia at supine position on orthopaedic radiolucent traction surgical table. The injured limb was kept in extension position by using traction, whereas the knee and hip of the healthy limb were flexed for the C arm X-ray machine fluoroscopy during operation. Closed reduction was achieved by adjusting the traction force, limb alignment and rotation. If X-ray showed good reduction, a 3–5 cm long incision proximal to the greater trochanter was created, and the greater trochanter vertex was selected to be the entry point of the guide wire. The guide wire was then inserted through the fracture line up to the distal femur. After checking that the guide wire is in position, we reamed the femur, selected the appropriate intramedullary nail to be inserted into the appropriate depth, placed the locking screws into the nail and then we checked the fracture reduction and internal fixation position again. If closed fracture reduction could not be achieved, a 1–2 cm long assisted incision was created. The fracture could always be reduced by poking, pulling and clamping, among others. If necessary, the fracture can be reduced and fixed by using the closed cerclage wire banding technique.
Locking plate: we use inverted distal femoral LISS plate (Synthese, Switzerland) as fixation. The patients were administered with general anaesthesia at supine position on orthopaedic radiolucent surgical table. A longitudinal incision (6−8 cm) was cut just distal of the greater trochanter. The fascia lata was sliced off, and the muscle fibre was separated. Subsequently, the greater trochanter was exposed. After choosing the appropriate LISS plate, the plate was reversed to be inserted through the proximal incision and then slid down distally beneath the muscle tissue with stripping of the periosteum of the lateral femur by using tools, such as periosteal elevator and hook. The plate was subsequently manoeuvred onto the distal fragment through a short distal incision, and proper placement of the plate and fracture alignment was checked by radiographs. K-wires were used for temporary fixation of the plate in the proximal and distal locations of the plate. After reduction and proper placement of the plate, the locking screws were used for stabilization. If the fracture could not be reduced by using the MIPO technology, the incision would be extended up to the distal site to better expose the fracture and direct fracture reduction. Autogenous iliac bone grafting is routinely performed in direct fracture reduction.
Postoperative treatmentThe passive joint functional activities and exercises were started the day after operation. Postoperative joint functional exercise on the bed lasted for 1 month, and partial weight-bearing functional training was started under the guidance of a doctor after 1 month. Postoperative examinations were conducted after 1, 2, 3, 6, 9 and 12 months after operation. Femoral X-ray examination was also conducted at each review; when necessary, femoral CT examination would be performed. Using the standard clinical and radiological criteria to evaluate fracture healing time and the hip Harris joint function score to assess hip joint function, we summarized the patients’ operation time, intraoperative bleeding volume, length of hospital stay, fracture healing time and hip function score and postoperative complications occurrence.
Statistical analysisThe operation time, intraoperative bleeding volume, length of hospital stay, fracture healing time and hip function score of the two groups were compared by t-test; the postoperative complication rate of the two groups was compared by chi-square percentage test. A value of p < 0.05 was considered statistically significant. SPSS software package (version 19, Chicago) was used to record and analyse the data.
ResultsIn the intramedullary nail group, the average follow-up time was 20.2 months (12–45 months). According to Seinsheimer fracture classifications, the group was divided into type II (3 cases), type III (13 cases), type IV (12 cases) and type V (3 cases). A total of 15 cases were treated with PFNA and 16 cases were treated with long reconstruction nail. The average operation time was 126 min (50–300 min), the average intraoperative bleeding volume was 258 ml (50–600 ml), the average hospitalization stay was 13.1 days (6–30 days), the average fracture healing time was 6.8 months (3–17 months) and the average hip function score was 82.5 points (66−93 points). During the last follow-up, internal fixations in two patients were removed. Fourteen patients underwent small incision-assisted reduction and two patients underwent closed cerclage wire fixation.
In the locking plate group, the average follow-up time was 19.4 months (12–30 months). According to the Seinsheimer fracture classifications, the group was divided into type II (4 cases), type III (8 cases), type IV (5 cases) and type V (3 cases). The average operation time was 161 minutes (50–360 minutes), the average intraoperative bleeding volume was 533 ml (200–1600 ml), the average hospitalization stay was 13.5 days (7–31 days), the average fracture healing time was 7.1 months (3–15 months) and the average hip function score was 81.9 points (68–92 points). During the last follow-up, internal fixations in two patients were removed. One patient underwent cerclage wire fixation and six patients underwent open reduction and autogenous iliac grafting.
Incidence of postoperative complications: 3 cases suffered from fracture non-union in intramedullary nail group, 1 case received augmentative plate treatment and autogenous iliac bone grafting 6 months after operation and 2 other cases received the original intramedullary nail removal and locking plate exchange treatment and autogenous iliac bone grafting because of intramedullary nail failure at 10 and 12 months after operation (Figure 1). One case showed delayed fracture healing, and autogenous bone grafting was performed 9 months after operation. Two cases in the locking plate group suffered from fracture non-union and they received the intramedullary nail exchange treatment and autogenous iliac bone grafting because of locking plate failure at 6 and 8 months after operation (Figure 2). One case showed delayed fracture healing, and autogenous bone grafting was performed 9 months after operation. During the last follow-up, all of the patients achieved bone healing and could walk with a load. No case suffered from wound infection, deep vein thrombosis and other complications. In addition, no other serious systemic complications occurred.
The results obtained from the two groups were compared and analysed, and only intraoperative bleeding showed significant difference (P < 0.05), whereas the operation time, hospitalization stay, fracture healing time, hip joint function score and postoperative complication rate showed no significant difference (Table1).
Discussion How to restore femoral medical support and avoid the fixation failure in intramedullary nail treatment in some difficult reduction fracturesIntramedullary nail offers more advantages in terms of mechanical properties and minimally invasive surgery; however, this treatment has a certain defect regarding the control of rotation, and a highly experienced and equipped physician should perform the treatment [12]. In the treatment of long spiral fracture, the intramedullary nail may lead to separation and displacement of spiral fracture fragment and fracture non-union [13,14]. The subtrochanteric area is subjected under high varus stress. If the posteromedial cortical is incomplete, then implant must bear high varus stress, which easily causes implant failure [1]. Intramedullary nail can minimize this problem, although if the posterior medial cortical defect lasts for a long time, the intramedullary nail will also fail. If closed fracture reduction is not ideal, we would create an assisted small incision for minimally invasive fracture reduction. MR Juan et al. [15] used small assisted incision to treat femoral subtrochanteric fracture by using intramedullary nail, and all of their 26 patients achieved bone healing. In our case, 14 patients were treated with assisted small incision, and the clinical results were satisfactory. In our series, two patients received closed cerclage wire banding for a spiral fracture reduction and fixation, and they showed successful bone healing. Using cerclage wire fixation to treat intramedullary nail by means of the closed wire technique is currently permissible, and this approach will not lead to non-union [16]. Therefore, in such femoral subtrochanteric fracture with difficult closed reduction, a small assisted incision could be used for fracture reduction, especially when recovering the femoral medial support. Closed cerclage wire can be adopted for fracture reduction and fixation when necessary. If reconstruction of the femoral medial support and the recovery of fracture reduction can be well achieved, intramedullary nail can generally provide satisfactory clinical results and will not lead to internal fixation failure.
Whether the locking plate will increase fixation failure and fracture non-union incidenceTraditional extramedullary fixation easily causes hip varus deformity, screw cutting, internal fixation failure, limb shortening and other problems [17]. By contrast, locking plate can well avoid these problems; thus, locking plate as extramedullary fixation is used widely to treat femoral subtrochanteric fracture. The inverted LISS plate can fit well to the femoral greater trochanter and can achieve minimally invasive reduction and fixation through the MIPO technology [18]. Kinast C et al. [19] compared the biological fixation and traditional open reduction and fixation in femoral subtrochanteric fracture, and they confirmed the obvious advantages of biological fixation over the traditional method in preventing fixation failure and promoting fracture healing. Biological fixation generally requires fracture alignment, prevention of obvious fracture angle and elimination of rotation but does not achieve anatomical reduction of fractures [20,21]. The LISS plate is placed on the periosteal surface and the screws are placed through small incision for fixation [22]. The LISS plate can efficiently preserve the blood supply and promote bone healing by a secondary means of healing with callus formation [23,24]. The proximal LISS plate should be placed at the medial-posterior part of the femoral greater trochanter to facilitate placement of the proximal screws into the centre of the femoral neck. The proximal screws should be adequately long to provide sufficient stability. Given the physiological curve of femur, the plate and femur may not match very well at the distal end of femur. An LISS plate should be placed to ensure that at least three bicortical screws can be fixed at the distal femur [7]. The posteromedial fracture fragment should also be reduced by using a lag screw and the clamp technique to reconstruct the femoral medial support; otherwise, internal fixation failure would easily occur [25]. The use of biological fixation and MIPO technology resulted in satisfactory clinical efficacy without internal fixation failure and non-union in our series. Therefore, the locking plate treatment should strictly abide by the "BO" concept, follow the principle of biological fixation and MIPO technique and protect blood supply rather than seek anatomical reduction through a wide range of stripping.
Summary of failures experienced in application of intramedullary nail and locking plateAnalysis of three cases of intramedullary nail failure: The first case displayed fracture non-union with numerous bone callus formation considering the intramedullary nail’s diameter was considerably small and its rotation is unstable. The 2 other cases displayed an obviously dislocated proximal femoral fracture fragment without medial femoral support. The missing medial femoral support resulted in fracture non-union and intramedullary nail failure. Therefore, in intramedullary nail treatment, the appropriate intramedullary nail diameter and length must be selected, and the treatment must focus on the restoration of the femoral medial support; otherwise, internal fixation failure will easily occur.
Analysis of two cases of locking plate failure: Two cases showed a serious comminuted fracture and were treated by open reduction. Although both of them achieved anatomical reduction of the fracture, plate failure still occurred resulting from fracture non-union caused by blood supply damage during open reduction. Therefore, the locking plate technique must follow the biological fixation and MIPO techniques; otherwise, this approach will easily lead to fracture non-union, resulting in internal fixation failure.
ConclusionWhen applied appropriately, the intramedullary nail and locking plate can both achieve satisfactory results in treatment of femoral subtrochanteric fracture, although intramedullary nail showed lower surgical injury and less bleeding. Intramedullary nail treatment must focus on fracture reduction and recovery of femoral medial support, whereas locking plate treatment must strictly abide by the concept of fracture biological fixation and MIPO technology.
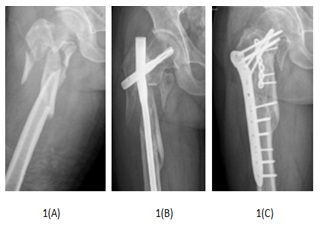
Figure 1: One patient suffered nail failure.
1(A): X-ray shows a serious fracture displacement and free medial femoral fracture fragment.
1(B): Fracture non-union and PFNA failure happened after long PFNA.
1(C): Bone union was achieved after locking plate revisionand autogenous iliac bone grafting.

Figure 2: One patient suffered plate failure.
2(A): X-ray shows serious fracture displacement
2(B): Fracture non-union and fixation failure happened after locking plate and reconstruction plate
2(C): Bone union was achieved after long reconstruction nail revision and autogenous iliac bone grafting.
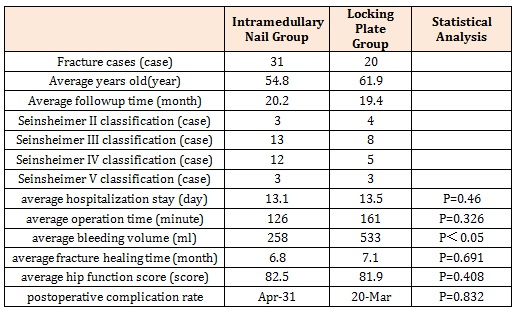
Table 1: Data of patients between two groups.
Chat with us on WhatsApp