Citation: Bernard J, et al. Do Hip Joint Positioning Affects the Maximal Voluntary Contraction of Gluteus Maximus, Gluteus Medius, TFL and Sartorius Muscles?. J Ortho Bone Disord 2017, 1(2): 000109.
*Corresponding author: Bernard J, IFMK Saint-Michel, Paris, France, Tel: +33 6 62 10 06 52; Email: sur.l a.seine@gmail.com
Background: Functional and clinical benefits from mini invasive total hip arthroplasty (THA) are widely known. Although it relieves pain and improves quality of life, literature reveals that gait and posturographic parameters of patients undergoing THA do not reach those of the general population. An electromyography study of the hip muscles involved in the surgery (Gluteus Maximus, Gluteus Medius, TFL, Sartorius) could provide some information. But the literature in the field of electromyography assessment of muscles shows discordant methodologies.
Purpose: The aim of this study was to develop a methodology to assess the maximal voluntary contraction (MVC) of Gluteus Maximus, Gluteus Medius, TFL, Sartorius muscle as a reference for normalization.
Methods: 30 young asymptomatic subjects participated in the study. Each realized 8 maximal voluntary contractions of the hip muscles in various joint positions on 3 sessions. Results: Statistical analysis showed no difference between the 3 sessions, and between the hip positions for hip abductors as well as for hip flexors to assess the MVC.
Conclusion: A single session and 1 test is enough to assess the MVC of hip abductors as well as for hip flexors.
Keywords: Total hip arthroplasty; Electromyography; Maximal voluntary contraction; Normalization
Total hip arthroplasty (THA) is the second most commonly performed surgical procedure, with an estimated number of more than one million operations each year worldwide [1]. Functional and clinical benefits from the anterior mini invasive approaches for THA are widely known [2,3]. However, Van Driessche et al. [4] showed there is a significant disturbance in the postural sway among patients who underwent THA, regardless of the surgical approach, although with some differences among the approaches when compared to the control group: the anterior and antero-lateral mini invasive approaches seems to be more disruptive of postural parameters than the posterior approach. These results imply that a lesion of the Sartorius and TFL muscles during the surgical approach could have a significant impact on posture. Thus, it seems important to study the activity of the muscles crossing the hip joint. An electromyography study of the hip muscles involved in the surgery (Gluteus Maximus, Gluteus Medius, TFL, Sartorius) could provide some information on the performance of the hip joint after THA during bipedal and unipedal stance. But there is no consensus on the method for studying hip muscles.
Literature in the field of electromyography assessment of muscles shows various methodologies [5-16]. Raw EMG data depend on several factors such as the skin impedance and the sensor location over the muscle belly. Normalizing the EMG signal allows inter group and intra group comparisons [11]. Nevertheless, very often the sensors location is not specified [17], and the reference for the normalization of raw data can be very different from a study to another [6,10,12]. This prevents from comparing data. The most common references for the study of hip muscles are based on the normalization with either a sub maximal muscle voluntary contraction [12], or the muscle activity during quiet bipedal stance [6], or a maximal voluntary contraction (MVC) [7,16].
Burden et al. [8] and Lin et al. [13] compared different methods for the EMG signal normalization, showing that only isometric and isokinetic contractions are reliable for MVC testing, without any difference in the mean of the EMG signal amplitude between these 2 methods. In terms of cost and time, manual testing for isometric MVC appears to be reliable and highly valuable for both asymptomatic subjects and patients with hip osteoarthritis or total hip arthroplasty [8,10,13].
In this context, as most authors do not specify which test they use for MVC testing [7,9,10,16], we investigated the impact of the hip joint positioning, and the learning effect on the Gluteus Maximus, Gluteus Medius, TFL and Sartorius muscles MVC.
We asked the following question: do hip joint positioning and learning of a MVC test affect the EMG signal during a maximal voluntary contraction of Gluteus Maximus, Gluteus Medius, and TFL and Sartorius muscles?
MethodsSixteen male and fourteen female persons between 18 and 30 years old voluntarily participated in the study (age: 21.2±2.4 years; height: 1,71±0,1 m; mass: 62,9±9,5 kg; BMI: 21,4±2). All the participants were free from any neurological, vestibular, musculoskeletal, cardio-vascular, respiratory, cognitive or psychiatric disease or impairment.
MVC TestingFor each muscle, MVC were obtained from manual testing [18] and the most common tests used in the literature [11]. Participants were asked to perform 8 MVC tests (2 for each muscle) with manual resistance placed distal to the femur (Figure 1):
We realized each MVC 3 times over one week, at the same schedule every day, controlling for activity levels in the preceding 24 h.
Data ProcessingFour bipolar surface electrodes (SX-230, Biometrics Ltd, UK), placed over the muscle bellies according to SENIAM recommendations [17] of Gluteus Maximus (GMax), Gluteus Medius (GMed), TFL and Sartorius (S) were used to record the electromyography (EMG). Signals were hardwardly band-pass filtered (cut-offs: 20 Hz – 450 Hz) and digitally sampled at 1000 Hz. Signal is offset by the rest EMG signal, smoothed with a sliding window at 50 Hz and rectified.
The EMG signal at rest is calculated from a dedicated record. The value used is the minimum signal on 1s after the 50 Hz sliding windows smoothing.
We chose the maximal mean of the signal over a 0.3 second interval as the MVC.
This MVC was expressed as a ratio of the EMG activity observed during the unipedal stance.
EMG unipedal stance had the same data processing (offset, 50 Hz sliding windowing, rectification) but the activity was expressed as the mean value of the rectified signal of a 10 seconds trial.

Verbal encouragements were used to enhance performance.
Statistical AnalysisNonparametric statistics were used to perform statistical comparisons. Mann Whithney U-tests were used both for comparisons between dominant and nondominant leg and for pairwise comparisons among the different tests. Comparisons among the 3 sessions were obtained with a Kruskal-Wallis H test. We considered a significant threshold of α=0.05. All the statistical analyses were carried out with the R software, version 2.14 (Bell Laboratories, Murray Hill, NJ, USA).
ResultsTable 1 shows the maximal value among the 8 tests for the 3rd session. We found no statistical difference (p<0.05) between dominant leg and non-dominant leg for the MVC.
Differences between testsFigure 2 shows for each muscle the percentage of maximal value depending on the MVC tests for the dominant leg.
As a result of what is observed on Figure 2, TGMd1 can be set as the most efficient test to determine MVC from hip abductors (GMx and GMd) and TS1 can be set as the most efficient test to determine MVC from hip flexors (TFL and S).
Table 2 describes the EMG activity (Mean±SD) for the dominant leg during the 3rd session as well as the statistical differences for each muscle between each of the 8 MVC tests and the most efficient test (TGMd1 for GMx and GMd, TS1 for TFL and S).
There is no statistical difference among the tests with hip abduction for determining MVC of hip flexors, or with hip flexion for the MVC of hip flexors regardless of the hip positioning.
Evolution of MVC between the 3 SessionsFigure 3 shows the boxplot for the evolution of MVC for each muscle, throughout the 3 sessions of MIVC testing, for the dominant leg.
MVC tests showed no statistical difference between the 3 sessions in the 1-week interval (p>0.05).
DiscussionTo our knowledge, this is the first study on EMG activity of hip muscles involved in THA. Because a reference for the normalization of raw EMG data is needed to enable inter and intra group comparison [8,10,11], and as most authors do not specify which test they use for MVC testing [7,9-11,16], we first wanted to develop a reliable methodology for assessing EMG activity of GMax, GMed, TFL and S muscle of young asymptomatic participants. We investigated 8 MVC tests based on the most common tests used in the literature [11], on 3 different sessions. We expected the hip positioning and the training to MVC tests would be determinant factors improving the EMG signal of MVC.
A limit from this study is the reference used for the normalization. The purpose of this study was to determine the best way to assess MVC of the GMax, GMed, TFL and S muscles, in order to use these results as a standard for the normalization of EMG signals in future studies.
For that purpose we still needed a reference for the normalization of MVC signals themselves, different from the MVC. We chose the EMG activity during the unipedal stance as the reference. Because our population is homogenous in age, height and weight, we can assume that the selected reference is reliable. But as previously shown by Burden et al. [8] and Lin et al. [13], this reference tends to show less statistical differences when compared to MVC.
Also, new data will complete this study in the future with patients who underwent THA with anterior, anterolateral and posterior mini-invasive approaches.
We were not able to confirm our work hypothesis: do hip joint positioning and learning of a MVC test affect the EMG signal during a maximal voluntary contraction of Gluteus Maximus, Gluteus Medius, TFL and Sartorius muscles? So we cannot affirm that hip joint positioning and learning of a MVC test affect the EMG signal.
The results from this study showed that there is no statistical difference between MVC tests to obtain the maximal EMG activity for hip flexors on one side and hip abductors on the other side. This means that MVC tests are reliable for MVC testing, regardless of the hip positioning.
We showed also that there is no statistical difference among the 3 sessions of MVC testing on the 1-week interval for each test. This shows that there is no learning effect from the training over the 3 sessions. This result is also showing that the tests are reliable to assess the maximal EMG activity of Gmax, GMed, TFL and S muscles.
Therefore we suggest using only 2 MVC tests on a single session to assess the MVC of the 4 muscles studied here among young asymptomatic subjects:
These tests are those described by Daniels & Worthingam [18] for muscle testing, respectively for GMd (TGMd1) and S (TS1).
We also can assume from these findings that even though EMG sensor placement and the normalization reference (MVC) is important for EMG data analysis [8,10,13,17], the way MVC is executed may not be a determinant factor. This enables comparing results from different studies as long as they use the same sensor placement as described in SENIAM recommendations [17].
ConclusionAs a conclusion, we answered negatively to our question: do hip joint positioning and learning of a MVC test affects the EMG signal during a maximal voluntary contraction of Gluteus Maximus, Gluteus Medius, TFL and Sartorius muscles?
However this study showed that we only need one test on a single session to assess the MVC of respectively hip abductors (GMAX, GMed) and hip flexors (TFL and S). This is an interesting result considering cost and time. The hip positioning does not appear as a determinant factor for MVC assessment.
This is a preliminary study that will allow analyzing GMax, GMed, TFL and S muscle activities in various conditions as postural assessment, with quick, simple, reliable and economic MVC normalization of the EMG signal, in young asymptomatic subjects. We believe this method is also transposable to other populations as HO or THA patients.

Figure 1: MVC tests.
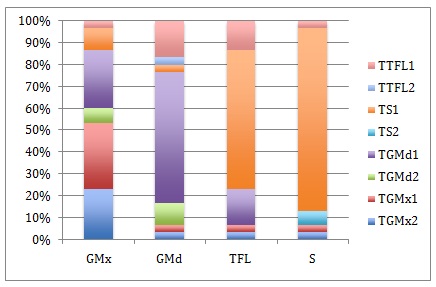
Figure 2: Percentage of maximal value depending on the MVC tests.
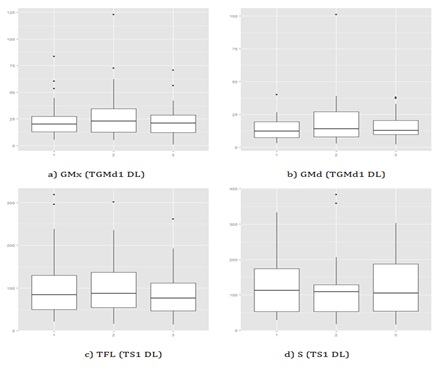
Figure 3: Evolution of MVC between the 3 sessions.
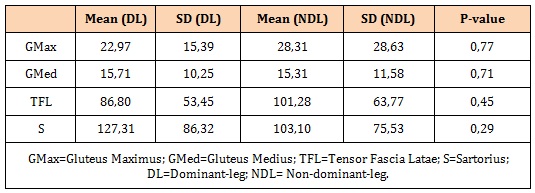
Table 1: Maximal value among the 8 tests (3rd session of MVC).
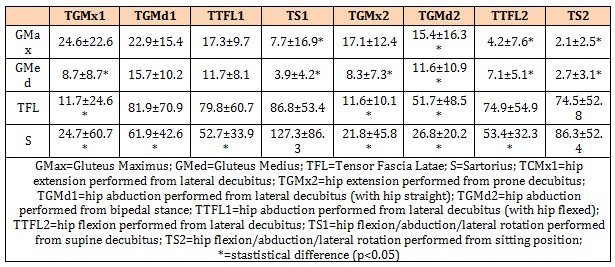
Table 2: EMG activity of each muscle for the 8 tests (3rd session of MVC).
Chat with us on WhatsApp