Citation: Federico A. Complications after De Quervain’s Disease Surgery. J Ortho Bone Disord 2017, 1(6): 000132.
*Corresponding author: Federico Amadei, Hand Surgery Center, Orthopedics Department Milano, Italy Tel: 3477600429; Email: amafede@libero.it
Surgical treatment of De Quervain improves symptoms, obtains good and quickly results with a local anesthesia procedure. Allows almost early return to work with few restrictions. It can provide complete pain and functional recovery and may offer a long-term solution. But it has a relative large number of complications, according to a review of the literature into 9 to 24 % of the cases. On this study we analyse the surgery complications in a randomized series of 20 patients treated by the same surgeon and with the same surgical technique (transverse skin incision and tenolysis).
In conclusions the surgery of De Quervain’s disease is a simple, safety and reliable technique but with a lot complications, particular the sensory branch of the radial nerve damage.
Keywords: De Quervain’s disease, complications, radial nerve
De Quervain disease was first described in 1895 as a disease that causes pain or tenderness in the first extensor compartment of the wrist at the level of styloid process of the radius.
This disease involves a thickening of both the tendons and the tunnel (extensor retinaculum) through which they pass and is produced by resisted gliding of extensor pollicis brevis (EBP) and the abductor pollicis longus (ABPL) that are responsible for bringing the thumb away from the hand as it lies flat in the plane of the palm.
There have been many entities related as cause of De Quervain the repetitive movements and forced postures are the most common related causes of this disease [1,2]. Some anatomical studies show myxoid degeneration, with disorganized collagen and increased cellular matrix. Nevertheless, some evidence of inflammatory phenomena has been found in retinaculum and an increase of it with the quantity of collagen structure.
De Quervain disease is considered a multifactorial disease [3-5]. Anatomic variations are been recognized as an important ethiopathogenic factor. Biomechanical factors like the number of fibro-osseous tunnels and compartments in the first extensor canal may be associated with a predisposition to de Quervain syndrome [6,7]. This entity has been described in mothers four to six weeks after delivery although the cause of these symptoms is not clear, having been attributed to both hormonal and mechanical causes. The most important ethiopathogenetics factors are also tenosynovitis and occupational risk factors.
The De Quervain disease is most common in women although the incidence varies depending on authors. It has been reported an incidence of 2.8 cases per 1,000 women vs. 0.6 cases per 1,000 men.
Most of population affected De Quervain are 30-50 years old. Many studies have shown that do not exist preference for the dominant hand and can be bilateral in the 30% of patient.
DiagnosisThe diagnosis based on clinical features of pain, the absence of trauma history and physical examination. The absence of bone radiologic signs and a negative carpometacarpal grind test associated with a positive Finkelstein's test are the usual findings [8-10].
Complementary diagnostics examines are sonography, MRI and X-ray [11,12].
The differential diagnosis was posed with the osteoarthritis of the thumb, the radial sensory nerve entrapment (Wartemberg syndrome), Ganglia, Crystalinduced arthropathies or Calcium hydroxyapatite deposits.
TreatmentThe goal of treatment is to decrease pain and increase the functionality/ability.
For this purpose there have been postulated several types of treatment: surgical, pharmacological and rehabilitative.
Most conservative therapies have limited results, splinting are one of the most popular conservative treatments as palliative [13,14]. Some authors obtain good performances with the use of ultrasound, cryotherapy and infrared rays or kinesiotaping [15]. Surgery is usually reserved to patients with persistent or severe symptoms despite conservative therapy [16].
The operations are performed under local anesthesia as ambulatory surgery. A 2-cm-long transverse skin incision is made on the radial styloid over the first extensor compartment and the dorsal retinaculum covering the extensor pollicis brevis is incised longitudinally [17,18]. As any surgery bleeding, infection and inability in postoperative period are possible. Other complication as poor quality and painful scar (Figure 1) [19].
Complications that limit normal hand function still occur despite advances in surgical techniques and therapy protocols. We must be careful not to injure cutaneous branches of radial nerve (Figure 2), otherwise a painful neuroma can appear. It’s very frequent a transient lesion of the radial nerve (50-60% of cases). Deficit of the superficial radial nerve (Figure 3). Persistent numbness in the web of the thumb, again owing to injury of the radial nerve branches. Subluxation of the tendon or incomplete release and persistence of symptoms are also possible [20-22].
ConclusionIn literature we found a complications rate into 9 to 24 % of the cases.
On this study we analyse the surgery complications in a randomized series of 20 patients treated by the same surgeon and with the same surgical technique (transverse skin incision and tenolysis).
In our experience we report 4 patients (20% of cases) with a temporary damage of the sensitive branch of the radial nerve (neuropraxia), with a symptomatologic output medium of 3 months. 1 Patient had a bad scar. No infections or hematoma are occurs in our series.
In conclusions the surgery of De Quervain’s disease is a simple, safety and reliable technique but with a lot complications, particulary the sensory branch of the radial nerve damage.

Figure 1: Scar after Surgery.
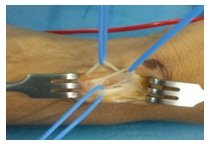
Figure 2: Sensitive Cutaneous Branches of Radial Nerve.
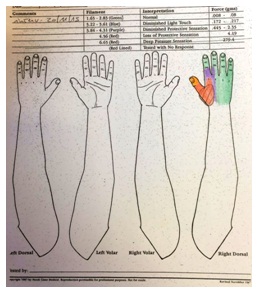
Figure 3: Sensibility Testing.
Chat with us on WhatsApp