
Citation: Yousif KI, et al. Perception of Ethical Principles by Hemodialysis Nurses in Khartoum, Sudan. Nurs Health Care Int J 2017, 1(2): 000110.
*Corresponding author: Kalthoum Ibrahim Yousif, College of Nursing Sciences, the National Ribat University, Burrie, Sudan, Tel: 0912172152; Email: kalthoumyousif@gmail.com
Background: In the nursing process the nurse must be able to make correct ethical decisions. This primarily requires knowledge of the basic ethical concepts and rules. Nursing curricula are not uniform in teaching nursing ethics and there is concern about applications of ethical principles during nursing practice.
Objectives: To determine the perception of ethical principles by hemodialysis (HD) nurses at dialysis centers in Khartoum state, Sudan.
Methods: A descriptive cross sectional hospital based study was used. Participants were nurses working in five HD centers from the period of July 2015 to February 2016. A total number of 120 dialysis nurses who agreed to participate in the study were included in the analysis. Data were collected through a self administrated questionnaire developed in accordance with current literature on nursing ethics and approved by a panel of five experts.
Results: All 120 nurses who agreed to participate completed the study. The respondents mean age was 34.8 years. Ethical principles studied included five ethical concepts; beneficence, nonmaleficence, autonomy, consent, and justice. Only about half of the participants (53%) reported that they formerly studied the principles of ethics during their nursing education. The scores for the principles of beneficence, nonmaleficence and justice were, in general, quite good. However, when analyzing the responses to questions related to patient autonomy, 60% of the nurses would not comply with patient's wishes if they contradicted with relatives wishes. Moreover, 30% of the nurses would leave decision making to relatives regarding care rather than patients. Nearly a quarter of the nurses did not seem to care for consent taking. This is alarming as patients’ autonomy and consent-giving did not seem to be well respected in dialysis centers.
Keywords: Ethics; Nurse; Nursing
Ethics is defined as the total of moral principles that form the basis of individuals’ behavior [1]. It is the philosophy of investigating, through analytical thinking, the values at the basis of relations between humans. This characteristic of analytical thinking distinguishes ethics from morals: ethics refers to a system of thought, while morals refers to the set of values that develop on their own with the rise and fall of different societies [1]. Ethics guide how people view the relevance of each decision made in the field of health, and is separated into two subcategories: theoretical and applied [2]. Theoretical ethics is concerned with the subject, meaning, and purpose behind philosophical ethics and examines its areas of responsibility. Applied ethics helps in deciding on what is right or wrong by laying out the liabilities that every health practitioner has towards his or her patients. Applied ethics teaches health practitioners the behavior that is in line with their own values. It assists in the decisions they must make, as well as their fulfillment with the profession [2]. The Florence Nightingale Pledge is acknowledged as the first ethical code for the medical profession [3]. It included important guidance rules for nurses. The Pledge reads as follows: “I will do all in my power to maintain and elevate the standard of my profession, and will hold in confidence all personal matters committed to my keeping and all family affairs coming to my knowledge in the practice of my calling. With loyalty will I endeavor to aid the physician in his work, and devote myself to the welfare of those committed to my care. I will abstain from whatever is deleterious and mischievous. I will not take or knowingly administer any harmful drug”. Since then, nursing has become increasingly acknowledged as a profession with unique values and principles [4]. However, the way in which the nursing profession changed over the years made it necessary to review and even amend these ethical codes. Thus, the American Nurses' Association (ANA, 1950) and the International Council of Nursing (ICN, 1953) reviewed the existing codes and established new versions. These "Nursing Ethics Codes" were presented with a new perspective on nursing, which demonstrated that nursing is an independent profession [4].
Nurses must be able to make correct ethical decisions. This primarily requires them to know the basic concepts, laws, rules, and other information related to the issue, and to seek continual improvement of their own nursing skills [5]. It is likely that the number of people with enough information about these codes is quite low despite being a very important subject especially in health-related fields [5]. We found no study describing the information and applications related to ethical principles of hemodialysis (HD) nurses in Sudan.
ObjectivesTo determine the perception of ethical principles by HD nurses at dialysis centers in Khartoum state.
Materials and MethodsA descriptive cross sectional hospital based study was conducted in five dialysis centers at Khartoum State from the period July 2015- February 2016. Participants were nurses attending these HD centers. Because nurses working in HD centers are from various States of Sudan, We considered that convenience sampling method would reflect a reasonable objective assessment. A total of 120 nurses, who had at least one year experience in dialysis, working at the five dialysis centers and who agreed to participate, were included in the study. Data were collected through a self-administrative questionnaire developed in accordance with current literature on nursing ethics [2,4,5]. The questionnaire consisted of 35 items. Six questions were on demographic information and 29 items contained five ethical principles: beneficence, nonmaleficence, autonomy, consent and justice. A panel of five experts in medical and nursing ethics evaluated, amended and finally approved the questionnaire as a reasonable tool for the research. Items’ answers were: “yes or no”. Ethical clearance to perform the research was obtained from the Ethics Board at The National Ribat University and the administrators of the assigned dialysis centers in Khartoum State. Furthermore, before the data collection, all participants were informed of the study procedure and their informed consent was obtained. The obtained data were analyzed using the Statistical Package of Social Sciences (SPSS) version 20.
ResultsA total of 120 nurses participated in the study. Their mean age was 34.8 years (range: 23-38) and only four (3%) were men. Half of the nurses were single and 15 of them (12.5%) had post-graduate degrees. The average work experience was 5.76 ± 6.42 years. Just over half of the nurses (53%) reported that they had studied nursing ethical principles during their Bachelor degree.
The percentages of perception of the ethical principles studied (beneficence, nonmaleficence, autonomy, consent and justice) by nurses during their daily practice are shown in Tables 1 to 4.
Table 1 shows the perception of ethical principles of beneficence and nonmaleficence during the daily nursing care. All of the nurses (100%) stated that human life must be protected, thus they integrated this into their practice. Although, most of the nurses (83.3%) did not make efforts to share their personal general knowledge with patients to build their confidence, yet 95.8% of them took extra effort to educate their patients about their medical problems. Moreover, 86.6% were prepared to postpone personal interests for the sake of their patient care. The majority of the nurses made efforts so that the patient does not experience maleficence due to nursing care or research applications. Nonmaleficence was observed by 96.7% of the nurses even if the patients were disrespectful to them.
Table 2 shows the nurses' perception towards patients' autonomy. With regards to patients' autonomy, 60% of the nurses were not keen to observe patients' wishes if they contradicted with relatives wishes. The majority of nurses (91.7%) stated that they would attempt to inform the patients and their relatives regarding their nursing care in a correct, adequate, and comprehensive manner. However, 30% of the nurses would leave decision making to relatives rather than patients.
Seventy five percent of the nurses respected patients' refusal of treatment but would discuss the issue with doctors and colleagues.
Table 3 shows nurses' perception towards consent taking. Seventy three percent of them would care about taking consent before nursing procedures. The majority (86.7%) would care for emergencies without waiting for consent.
Table 4 shows nurses' perception of justice and equity during their practice. Ninety percent of the nurses would not prioritize patients that were related or acquainted to them. Similarly, 90% of the participants stated that they would provide nursing care without discrimination between individuals because of differences in race, language, religion, or political view.
DiscussionThe ethical principles established by modern medical ethics fall into five practical categories: beneficence, nonmaleficence, autonomy, consent and justice [1]. Beneficence: is based on providing benefit to the patient. It provides guidance to nurses in prioritizing patient beneficence, doing good, and avoiding maleficence [6]. Non-maleficence: is the principle based on preventing doing harm to the patient [6]. Autonomy: is the principle that dictates the ability of the individual to make decisions about health or work according to the values, beliefs, and expectations independently. This principle is based on the principle of self determination, and aims to protect human dignity [7]. This principle also refers to respecting the privacy of the patient during treatment and in any instance that the nurse is involved with the patient. The most significant reflection of the principle of autonomy in the field of health is informed consent [7]. Justice: refers to treating each individual fairly. It emphasizes the importance of being careful that resources at hand are equally shared (equity), particularly when deciding on treatments [8,9].
Over half of the nurses participating in this study (53%) reported that they had formally studied nursing ethical principles during their Bachelor degree studies. Nevertheless, all the nurses stated that they would observe the five principles of ethics in their practice.
The current perception of ethical principles by nurses in this study was acceptable for the principles of beneficence, non-maleficence and justice (over 90% of the nurses would observe applying these principles).
It is comforting that most nurses (86.6%) stated that they would postpone their personal interests for the sake of their patients' care (beneficence). Ninety six percent of nurses would provide care to patients even if they were disrespectful to them (nonmaleficence).
There was concern about caring for patient autonomy with respect to decision making and giving consent independently: 60% of the nurses would not comply with patient's wishes if they contradicted with relatives wishes.
Moreover, 30% of the nurses would leave decision making to relatives regarding care rather than patients. This is alarming as patients’ autonomy did not seem to be well respected in dialysis centers. Seventy five percent of the nurses respected patients' refusal of treatment, but this issue should be discussed with the doctors and the nursing staff.
Obtaining consent from patients during nursing practice was cared for by only 73% of nurses. Nearly a quarter of the nurses did not seem to care for consent taking. In situations with minors or incompetent patients the lawful guardian would be approached for consent by 90% of nurses. Similarly, 90% would care for emergencies without waiting for consent.
ConclusionIt is apparent that a reasonable number of nurses working in HD centers in Khartoum act in compliance with the major ethical principles. However, there is a need for appropriate education of ethical codes in detail. Emphasis needs to be added on the importance of patient autonomy especially with regards to decision making and independent consent to various procedures.
AcknowledgementI am indebted to all the nurses who contributed to this study and availed their time and cooperated patiently with the researcher's requirements.
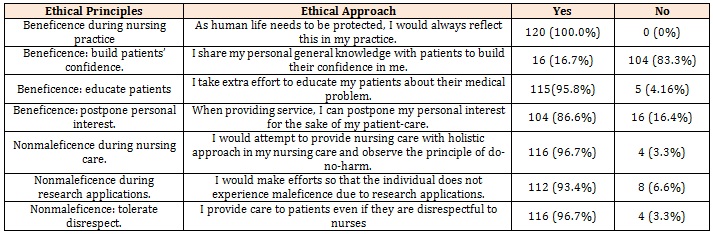
Table 1: The perception of ethical principles of beneficence and nonmaleficence by nurses during daily practice.
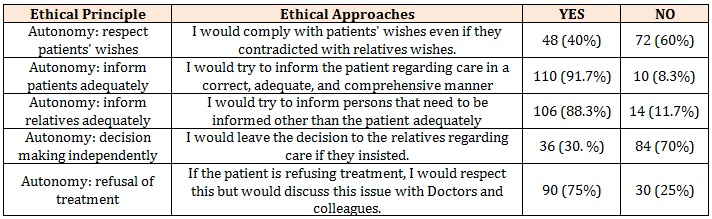
Table 2: The perception of nurses' to the ethical principle of patients’ autonomy during their daily care.
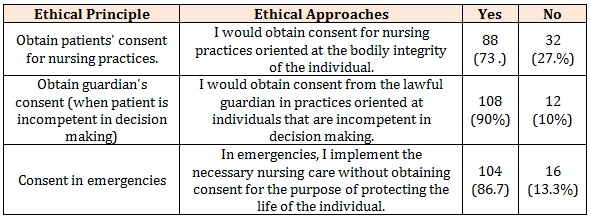
Table 3: Distribution of nurses' perception of ethical principle of obtaining patient consent during daily care.
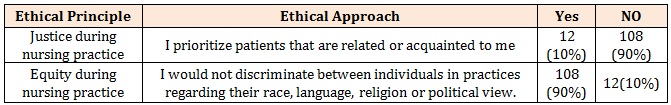
Table 4: Distribution of nurses' perception of ethical principles of justice and equity during their daily care.
Chat with us on WhatsApp