Citation: Shao AG, Kahabuka FK, Mbawalla HS. Children’s Behaviour in the Dental Setting according to Frankl Behaviour Rating and their Influencing Factors. J Dental Sci 2016, 1(1): 000103.
*Corresponding author: Febronia Kokulengya Kahabuka, Department of Orthodontics, Paedodontics and Community Dentistry, 3rd Floor Room 303, P.O. Box 65014, Dar es Salaam, Tanzania, Tel:+255-22-2151135; Email: kokukahabuka@yahoo.com; fkahabuka@muhas.ac.tz
Background: Execution of eminence oral health care to child dental patients to a large extent depends on the child’s behaviour during a dental visit. This study assessed children’s behaviour using Frankl behaviour rating scale and examined the influencing factors.
Methods: A cross sectional study among 222 children aged 3 to 12 years attending a university dental clinic for routine dental care. They were interviewed on social background; their behaviours were observed then rated and clinically examined. Children’s behaviour was reported as mean, differences between groups in prevalence scores and odds ratio, OR. The level of statistical significance was set at p≤0.05.
Results: In general 48.6% of the children had a mean score of positive behaviour. More than 50.0% of the children who were six years or older, attending primary school, whose parents had secondary education or higher, displayed positive behaviour compared to their counterparts. A child who had not started school was less likely to have positive behaviour with OR 0.21(0.04, 0.99) for negative, 0.09(0.02, 0.42) for positive and 0.05(0.01, 0.44) for definitely positive. Children who visited the clinic due to pain were less likely to behave definitely positive OR 0.14(0.03, 0.81) while those who were cooperative at a previous dental visit were more likely to behave both positive and definitely positive, OR 4.26(1.01, 17.96) and 9.45(1.68, 53.39), respectively.
Conclusion: Most children behaved positively and their behaviour was influenced by socio-demographics, family socialization and environment related to dental settings.
Keywords: Behaviour rating; Dental setting; Frankl behaviour rating scale
Human behaviour is a manner of conducting oneself. From a medical point of view it is any response emitted by or elicited from a human [1]. Children's behaviour depend on the level of development, age, the context in which the behaviour occurs, the child's own particular family values and expectations, cultural and social background. Children are said to learn set of behaviours and use them successfully to help them cope with difficult or anxiety-inducing situations. In the dental setting, children will naturally use these coping strategies, some of them will be helpful while others not [2]. In paediatric dental service provision point of view, to a large extent execution of eminence oral health care to child dental patients depends on the child’s behaviour during a dental visit. In other words, children’s dental anxiety and fear is considered to be the main barrier for successful completion of dental treatment [3]. Therefore, as much as it is essential for dentists to know how to manage the children’s behaviour in the dental settings, it is imperative to know the factors that influence the behaviours. These factors could be social, dental, child’s attributes or environmental. Social factors include: parental level of education [4,5], family social economic status, [6] family life, religious influence and education [7], socialization and information received from others [8-11]. The dental factors comprise the child’s past dental experience, reason for dental visit, child’s cooperation at previous visits, the dental team [4,12], type of dental settings, effectiveness in behaviour management and the nature of the dental procedure [13]. Child’s attributes include; psychological and behavioural characteristics, temperament and age [14-18].
Assessment of the child dental patient's behaviour in a dental setting helps to alert the dental team of a particular patient’s anxious level and facilitates planning for proper behaviour management. Additionally, proper assessment of children’s behaviour helps the dentist to plan appointments and render effective and efficient dental treatment, as Sharma & Tyagi reported [19]. Furthermore, behaviour rating facilitates prediction of children’s behaviour thus it might help in selecting appropriate behaviour management technique to be used in a particular child or type of children. Appropriate use of management techniques can improve the child’s behaviour in subsequent dental visits.
Behavioural rating scales have been the most commonly used indices of children’s responses to dentistry. The advantage of rating scales includes; ease of administration and conceptualization [20]. A variety of behaviour rating scales have been used to assess and evaluate children’s behaviour in the dental settings [21- 25]. Of these, Frankl Behaviour Rating Scale has been widely validated and accepted for use and was adopted in this study. The scale was conceived by Frankl et al. [21] who classified child’s behaviour into four groups according to the child’s attitude and cooperation or lack of cooperation during dental treatment.
Behaviour rating in the dental settings has been done in several parts of the world but reports in the African location are scarce. In Tanzania, a large proportion of dental care is provided at public dental facilities, with nearly all being located within hospital settings. Furthermore, majority of the clients are walk-in patients often seeking dental consultation due to pain. These scenarios add on the negative influence of children’s behaviour in the dental settings thus a need for dental practitioners to have mechanisms for behaviour management. A recent study [26] has demonstrated satisfactory Tanzanian dental practitioners’ awareness and application of behaviour management techniques but none has assessed children’s behaviour nor factors associated to the behaviours. Therefore, the objective of this study was to assess children’s behaviour using Frankl behaviour rating scale and examine the influencing sociodemographics, social and dental factors.
Materials and MethodsThis was a descriptive cross sectional health facility based study that was conducted at a university paediatric dental clinic in Dar-es-Salaam, Tanzania. A minimum sample size of 214 children was estimated to be satisfactory based on the assumption that; proportion of children with uncooperative behaviour in the dental setting is 50%, using absolute precision of 0.05 and 90% confidence interval. All children aged 3-12 years old seeking dental services as outpatients at the clinic between December 2014 and February 2015 were eligible to take part in the study provided they were otherwise healthy, without vivid psychological or intellectual impairment. To attain the required sample size every child meeting the inclusion criteria who sought dental services on the days of the study was recruited, ultimately 222 children, a response rate of 104% was attained.
Data collection was done through interview using a structured questionnaire designed for the purpose of this study, observation and recording of the child’s presenting behaviour and clinical examination for dental caries. The questionnaire was pre-tested to 5% of expected sample size before embarking to data collection. The results of the pilot testing were used for content and language editing. The questionnaire inquired on parents’ and children’s socio-demographic characteristics (age, sex, child’s schooling status, having siblings, parents’ highest level of education and employment status), socialization and environment related to dental visit and settings (information given prior to dental visit, use of phrases for dental/hospital being unfriendly to shape the child, reason for dental visit, frequency of dental visits, cooperation at previous dental visit(s), attending dentist’s level of training and working experience).
The observation of children’s behaviour was done by one of the authors (AGS), who was not involved in treating the child. The behaviour was assessed at three points; as the child entered the dental clinic, during clinical examination and during treatment. The observer trained on rating the child’s behaviour using a standardized and clinically accepted Frankl behaviour rating scale [21]. The scale consists of four behaviour categories; category 1 is definitely negative which means refusal of treatment; crying forcefully, fearful, or any other evidence of extreme negativism. Category 2 is termed negative, it is characterized by reluctance to accept treatment, uncooperative, some evidence of negative attitude but not pronounced that is; sullen, withdrawn. Category 3 is termed positive; whereby the child presents with acceptance of treatment; at time cautious; willingness to comply with the dentist, at time with reservation, but follows the dentist’s directions cooperatively. Finally, category 4 is termed definitely positive; characterized by good rapport with a dentist, interested in the dental procedures, laughing and enjoying the situation. Clinical examination for dental caries was done by the attending dentist in the normal clinic setting through visual inspection utilizing a mouth mirror and artificial light. The children’s caries status documented on the day of the study was extracted from the patient’s records and scored as 0 = Sound, 1 = decay, 2 = decay with pulp involvement, 3 = filled with decay, 4 = missing due to caries.
Data entry and analysis was done using Statistical Package for Social Sciences (SPSS) computer program version 20. The data were transformed for analysis purposes as follows; child’s age into younger than six years and six years or older, schooling status into not schooling or nursery school and primary school, having siblings into with or without siblings, parents’ highest level of education into less than secondary education and secondary education or higher, and employment status into self-employed or employed. Furthermore, transformation was done for information given prior to dental visit into a visit for tooth removal or for dental consultation and help, reason for dental visit as due to acute dental pain or dental complaint without pain, frequency of dental visits was categorized as being first visit or had a previous dental visit, cooperation at previous dental visit into cooperative or uncooperative and finally attending dentist’s level of specialization as general practitioner and paediatric dentistry resident or specialist. The child’s behaviour in the dental setting as a mean score was computed by summing up each child’s score on entering the dental clinic, during clinical examination and during treatment divided by three. Dental caries in deciduous and permanent dentition was computed as a summation of all the teeth with caries experience (decayed, extracted/missing and/ or filled due to caries). The sum of teeth with caries experience was further grouped into those without caries (caries free) and with at least one decayed, extracted/missing and/ or filled tooth.
Univariate analyses were done to generate frequencies of children’s behaviour on entering the dental clinic, during examination and dental treatment. The child’s mean behaviour scores were generated and used for further analysis. Bivariate analyses using chi- square statistics was done to assess the association between children’s behaviour in the dental setting with the sociodemographics, social and dental environmental factors as well as dental caries experience. Those factors that were statistically significantly associated with the children’s behaviour in bivariate analyses were taken into multivariate analyses, in this case multinomial logistic regression and presented as Odds Ratio (OR) and 95% Confidence Interval (CI). The level of statistical significance was set at p≤0.05.
ResultsThe study involved 222 children aged 3 to 12 years (mean age of 7.15, SD 2.64). Children aged six years or older were 69.4%, males were 51.4%, those who had siblings were 86.9% and those who have not started school or were attending nursery school were 43.2% of the participants. Thirty percent of mothers and 20.7% of the fathers had lower than secondary school education, while 42.3% of the mothers and 57.7% of the fathers were employed (Table 1).
On entering the clinic, equal proportions of children displayed negative (37.8%) and positive (37.4%) behaviour while during dental treatment more than half (51.8%) showed a positive behaviour. The proportion of children who displayed negative behaviour decreased from 37.8% on entering the clinic to 30.6% during examination and to 27.5% during treatment. The children displaying positive behaviour increased from 37.4% on entering the clinic to 49.1% during examination and to 51.8% during dental treatment, (Figure 1). Overall, 48.6% of the children had a mean score of positive behaviour (Figure 2).
(Table 2) presents the factors considered to have influence to the child’s displayed behaviour during dental visit. More than half of the children (52.3%) were told that they were being sent to the dental clinic for tooth extraction and 66.2% of the families reported to shape their children’s behaviour by using phrases about hospitals and dental clinics that may be unfriendly to the child such as; “if you will not behave, you will be sent to a dentist”. Most children (62.2%) attended due to acute dental pain, 22.1% were visiting a dentist for the first time, and 66.7% were reported to show a negative behaviour at their previous dental visits. Majority of the attending dentists were general practitioners (81.1%) and had a working experience of less than one year (79.7%). More than three quarters (77%) of the children had at least one of their deciduous teeth decayed, filled or extracted due to caries. The percentage was 9.9 in the permanent dentition. Most of the children (70.3%) were attended during morning sessions.
The socio-demographic characteristics that showed statistically significant relationship with children’s behaviour were; child’s age, child’s schooling status, and parents’ level of education. Whereby, more than half of the children who were aged more than six years (54.5%), attending primary school (58.7%), whose mother’s and father’s had secondary education or higher, (54.2%) and (52.8%) respectively, displayed positive behaviour as compared to their counterparts (Table 3). All the sociodemographic variables that showed statistically significant associations with child’s behaviour in bivariate analysis (child’s age, child’s schooling status and parents’ level of education) were taken into adjusted multinomial analysis. Only child’s schooling status maintained the statistical significant association with the child’s behaviour in the dental settings (p < 0.05), in a way that a child who had not started primary school was less likely to have positive behaviour with OR 0.21(0.04, 0.99) for negative, 0.09(0.02, 0.42) for positive and 0.05(0.01, 0.44) for definitely positive (Table 4).
Both family related factors that is, information given to the child prior to a dental visit and family use of phrases about hospitals and dental clinics to shape their children’s behaviour were significantly related to children’s behaviour. Children who were informed that their visit is for consultation (53.5%) and those from families that do not use unfriendly phrases about hospital/dental clinic to shape their children’s behaviour (61.3%) had positive behaviour compared to their counterparts. Dental environmental factors that were statistically significantly associated with displayed children behaviour were; reason for the dental visit, frequency of dental visits and child’s cooperation at the previous visit. Children whose reason for visit was not associated with pain (53.8%), who had previous dental visits (52.0%) and those who were cooperative at their previous dental visits (61.5%) displayed positive behaviour as compared to the rest (Table 5).
Four socialization and dental environmental factors that showed statistically significant associations with child’s behaviour in bivariate analysis were taken into adjusted multinomial analysis. Reason for dental visit and child’s cooperation at the previous visit retained the significance association with child’s behaviour. Children who visited the clinic due to pain were less likely to behave definitely positive OR 0.14(0.03, 0.81) while those who were cooperative at a previous dental visit were more likely to behave both positive and definitely positive, OR 4.26(1.01, 17.96) and 9.45(1.68, 53.39), respectively (Table 6).
Larger proportions of children displaying positive (54.9%) and definitely positive (21.6%) behaviour were caries free in the deciduous dentition compared to the ones with caries. Correspondingly, larger proportions of children displaying definitely negative (12.3%) and negative (35.7%) behaviour had caries in the deciduous dentition compared to their counterparts, (Figure 3). These differences were statistically significant (p<0.001). The low percentage of caries (9.9%) in the permanent dentition under-powers the bivariate results and hence are not presented.
DiscussionThe participants of this study were; mainly aged six years and beyond, boys and attending primary school. A good number of their parents had secondary school education or beyond and were employed. This implies that children at school age and having parents with medium/high social status (educated and employed), are likely to report their complaint to their parents who take the required action.
Most of the children who participated in the current study displayed positive behaviour (Frankl behaviour rating scale 3) during their dental visit. The positive behaviour seen in this study may be explained by African nature of being positive tempered as stated by Aminabad et al. [18] that temperament seem to act as a predictor of child behaviour in the dental setting. Similarly, Sachio et al. [27] in Japan and Sharath et al. [28] in India reported positive behaviour to be dominating. The proportion of children displaying negative behaviour decreased from entering the clinic to during treatment while those showing positive behaviour increased from entry to treatment. Perhaps, on entry children are not certain on what is to happen to them. Subsequently, upon application of behaviour management techniques in the course of history taking and clinical examination, some children’s behaviour change from negative to positive although only a few changed to definitely positive. These findings are in agreement with those of Roberts et al. [2] that in the dental settings children naturally use their coping strategies to help them deal with dental surroundings. A similar situation was reported by Sharath et al. [28] and Sharma & Tyagi [19] who stated that children showed improvement in their behaviour with every subsequent visit.
Social and dental environmental factors that are thought to negatively influence children’s behaviour were prevalent among the studied population in a way that more than half are given negative information prior to dental visits and two thirds of the parents use unfriendly phrases to shape children’s behaviour. This could be explained by the fact that, there exists a notion among Tanzanians that treatment of a toothache is extraction hence parents share the notion with their children. Furthermore, using negative phrases about dentistry may be a result of many communities considering dental treatment scary [29,30].
Nearly 80% of the studied children had been to a dentist before; probably some patients were referred from primary health facilities for the specialized care provided at the study facility. On the other hand, some patients may have been recalled for follow-up. A high percentage of participants who have been to a dentist before in the current hospital study is unlike a common finding in the African settings. Previous studies in the region showed that very few children and adults visit dental clinics, majority doing so on emergency basis and that most people walk with unattended dental conditions due to pain [31-33].
Parents’ report that two thirds of the children (67%) were uncooperative at previous visits may be a result of different means of parents to assess children’s cooperation which could have resulted into overestimation. Most of the attending dentists (81%) were general practitioners and nearly 80% had less than one year of working experience, majority were intern dentists and postgraduate students since the facility is under a teaching hospital. A substantial proportion of children had caries in the deciduous dentition, an expected finding because previous studies [34,35] have shown that most dental patients visit dental clinics due to caries related problems.
Most of the older children behaved positively and definitely positive compared to the younger children. Older children are more likely to be emotionally mature to understand things and tend to cope to new places. This finding is supported by Aminabadi et al. [36] who reported that among children, a more positive behaviour can be expected as the age increases. Children who were attending primary school were less likely to behave negatively. Possibly their attendance to school offer them opportunity for secondary socialization such that being in a new environment, in this case a dental clinic, and meeting new people is no longer strange.
Children whose parents had secondary education or above, displayed positive behavior than their counterparts indicating that parents’ education thus parenting style could have influenced children’s positive behaviour in the dental setting. Our findings are in line with those of Kamran et al. [37] who reported that there was a trend for children belonging to parents with college/university education to behave positively. On the other hand, those who were informed that their visit is for consultation and those from families that do not use unfriendly phrases about hospital/dental clinic to shape their children’s behaviour had positive behaviour compared to their counterparts. These observations imply that when children are given positive information about dentistry, are likely to behave positively during dental treatment. However, our findings are different from those of Folayan & Idehen [38] who found that there was no significant differences between the behaviour of children who received positive compared with those who had negative information.
Factors pertaining to children namely; reason for visit associated with pain, not having previous dental visit, having caries in their deciduous dentition and being uncooperative at previous dental visits significantly associated with negative behaviour. Furthermore, the adjusted multinomial analysis of the current study revealed that, it was unlikely for the child to behave definitely positive if the visit was related to pain. Usually, pain due to caries is the main reason for young children’s visit to dental clinics. On the other hand, the child who was said to be cooperative at the previous dental visit was more likely to behave definitely positive. Apparently, pain increases the child’s apprehension which on its own promotes negativity and anxiety that may contribute to a child’s negative behaviour. In similar reasoning, a child who was not cooperative at previous dental visits is expected to be negative unless intervention has been done. Although visiting a dentist before may be thought to contribute to children’s negative behaviour, if the visit was pleasant, a child may behave well at subsequent visits. This was shown by Suprabha et al. [12] in their study, that children who had pleasant experience at previous visits and had visited a dental clinic before were cooperative in the dental setting.
Study LimitationsInterpretation of the current findings should be done bearing in mind that; there could have been type II error as a result of inconsistency in observing and recording children’s behaviour over a period of time (reliability) that could have been reassured through reliability testing. Intra-examiner agreement examinations were not done due to the nature of the dependent variable (observed child’s behavior) that could not allow repeated examination. This could have contributed to overestimation of children who behaved positively. Furthermore, the wide range in 95% CI observed could be explained by a hidden nature of the sampling design where in a lot of ways the study was conducted under a pseudo-cluster sampling and the design effect was not taken under consideration.
Conclusion and RecommendationsMost children behaved positively, the proportion of which increased from the time the child entered the clinic to treatment. Child’s behaviour was influenced by his/her age, schooling status, parents’ level of education, reason for child’s visit, having previous dental visit and cooperation at previous visits. Information given to the child prior to dental visit and the practice of families to use unfriendly phrases about hospital/dental clinic also influenced children’s behaviour.
It is recommended that dentist should strive to make children’s dental visit pleasant and motivate parents to seek early dental consultation, give their children positive information before dental visits and avoid using unfriendly phrases about hospital/dental clinics.
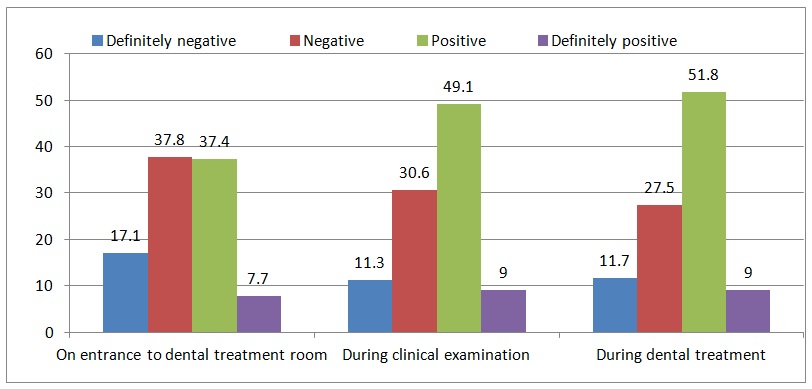
Figure 1: Frequency distribution of children's behaviour assessed at various stages in dental clinic
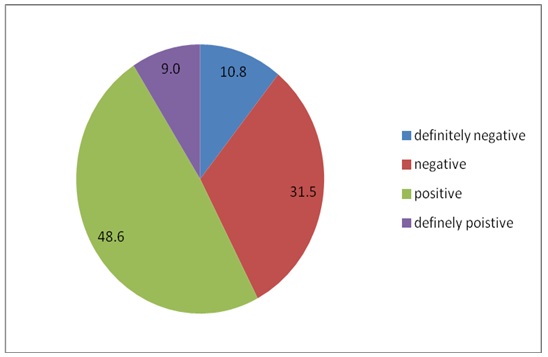
Figure 2: Mean score of participants' behaviour according to Frankl Behaviour Rating scale
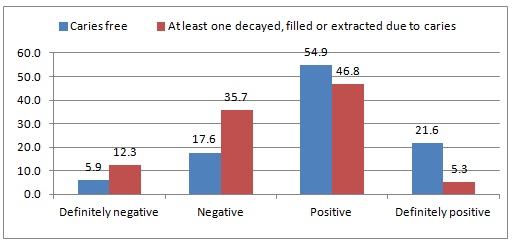
Figure 3: Participants' behaviour according FBRS by caries experience in the deciduous dentition
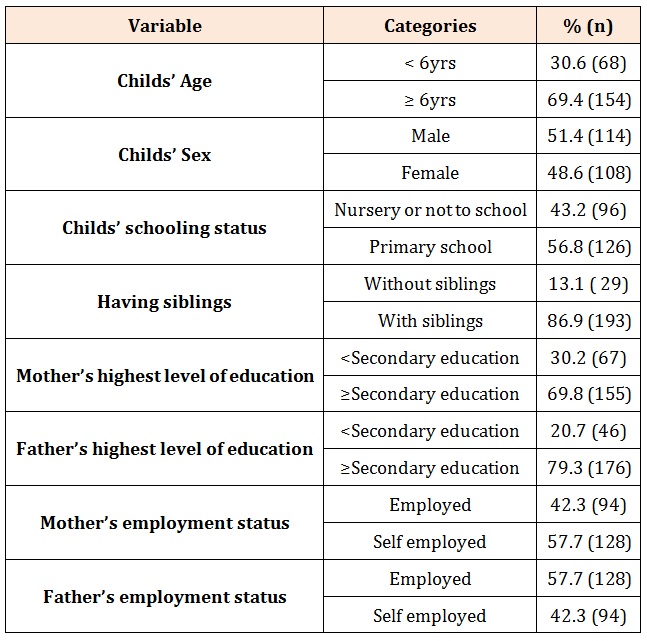
Table 1: Frequency distribution of participants’ socio-demographic characteristics

Table 2: Frequency distribution of participants’ socialization, dental environment and dental caries experience.
* 17 children had missing information on child’s behaviour at previous visits.
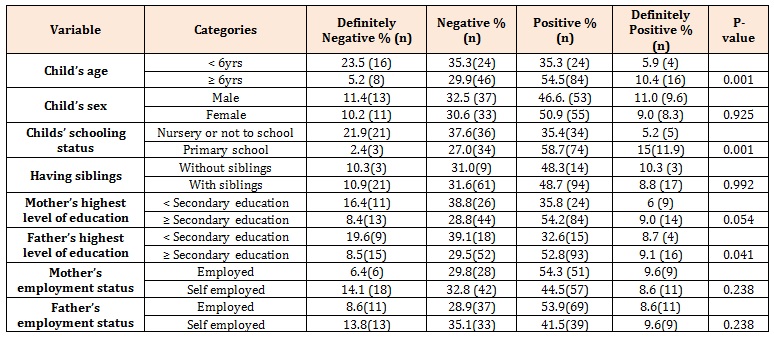
Table 3: Participants behaviour according to FBRS by socio-demographic characteristics.
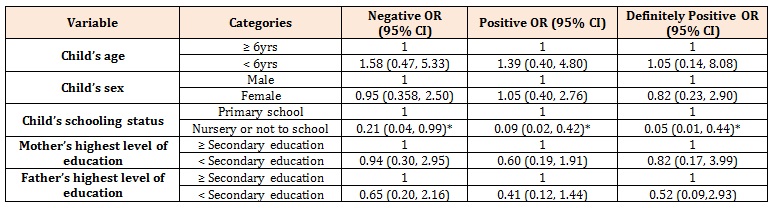
Table 4: Adjusted multinomial logistic regression in OR (95% CI) for children’s behaviour according to sociodemographic characteristics
* p≤0.05
Note: The reference category is definitely negative
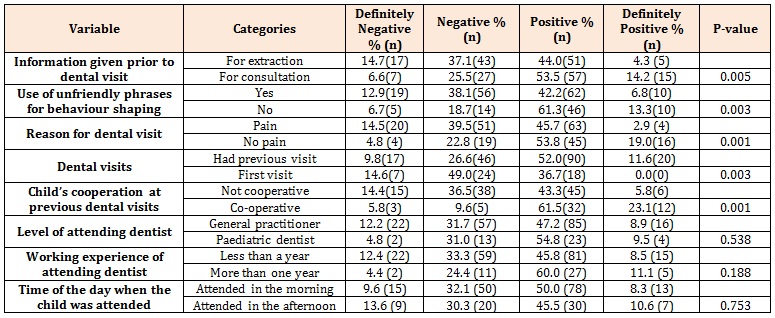
Table 5: Participants’ behaviour according to FBRS by socialization and dental environmental factors
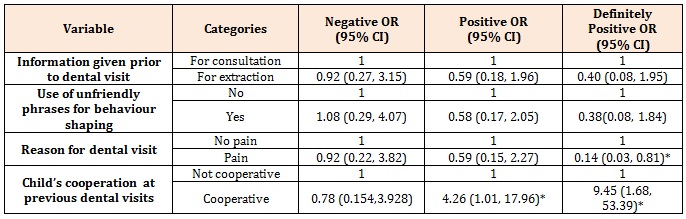
Table 6: Adjusted multinomial logistic regression in OR (95% CI) for children’s behaviour according to socialization and dental environmental factors.
* p≤0.05Note: The reference category is definitely negative
Chat with us on WhatsApp