Citation: Abdul Cader SH, et al. A Comparative Study of Efficacy of Different Surgical Management Options and Hearing Outcome in Children with Otitis Media with Effusion. Otolaryngol Open Access J 2016, 1(3): 000114.
*Corresponding author: : Segana Hasan Abdul Cader, Specialist ENT surgeon, Sur Hospital, Ministry of Health, Sultanate of Oman, Post Box 1004, Postal Code 411, Email: dr_shac@yahoo.com
Introduction: Otitis Media with Effusion (OME) also known as Secretory Otitis Media or glue ear is one of the commonest causes of preventable deafness among Paediatric population. The most common cause being Eustachian tube dysfunction. There are no constant surgical procedures involved to treat OME. Possible combinations of various surgical modalities include Myringotomy with or without insertion of ventilation tube either alone or with adenoidectomy or tonsillectomy or both.
Aims and Objectives: To study the epidemiology, clinicoaudiological profile and radiological characteristics as well as treatment outcome of children less than 12 years old diagnosed with Otitis Media with Effusion (OME) and to assess the effect of four different surgical treatments for glue ear (Myringotomy with grommet insertion, Myringotomy with Grommet plus adenotonsillectomy, Myringotomy with grommet plus adenoidectomy alone, Myringotomy with grommet plus tonsillectomy alone), on improvement in hearing.
Materials and Methods: The study was conducted from January 2011 to January 2015 in Sur Ministry of Health Hospital and was performed upon 150 children up to 12 years old who were diagnosed as OME. Complete clinical, radiological and audiological investigations were performed. All the patients received medical treatment and were subjected to surgical management and the results were obtained. The patients were followed up 6 weeks, 3 months and 6 months postoperatively. Postoperative PTA was obtained and hearing outcome was plotted.
Results: The prevalence of OME in our study was mostly males between 5-7 years and mostly presented with hearing loss of moderate degree. The commonest otoscopic finding was retracted tympanic membrane. Tympanometry showed B tracing in 78.5% patients. The commonest radiological finding was a grade 3+ adenoid hypertrophy in 42 patients. Most of them received Nasal steroid spray as a form of medical management, surgical modality was started in resistant cases of medical management and a combination of various surgeries performed shows that Myringotomy with grommet insertion and adenoidectomy alone relieved the OME and the Air Bone gap shows that the hearing outcome was better in a gradual follow up period.
Keywords: Glue ear; Otitis media with effusion; Adenoidectomy; Tonsillectomy; Adenoidectomy; Grommet insertion
Otitis media with effusion (OME) or glue ear in children is one of the most common conditions encountered by the practising otorhinolaryngologists in the Sultanate of Oman. It’s one of the most common early diseases of childhood with a peak incidence at the age of 2 years [1], and is the commonest reason for elective surgery in childhood. As many as 90 percent of children will have at least one episode of OME by age 10. Many episodes are short-term and transient; they do not recur or recur infrequently. A third of them will have the attack without any premonitory symptoms and these have been called “silent” otitis media [2]. Incidence varies according to geography and race with preponderance to Blacks. These variations may be genetic but anatomical skull base and Eustachian tube variations may play a significant role. In general an incidence of 8-50% is acceptable.
The incidence decreases with increasing age i.e. from 40% at two years to 1.4% at 11 years [3]. Environmental factors such as pollution, seasonal variation with a peak in winter and recurrent upper respiratory tract infections are usually associated with high incidence [4]. Socio-economic factors that cause crowding, poor hygiene and diet, poor education, inadequate nutrition, poor medical services and healthcare facilities and overcrowded poor accommodation seem to increase the incidence and severity of the disease [5]. The increase in the incidence of the disease in the last two decades seems to decrease due to improvement in health services, otological services, screening programs, awareness by parents and teachers and improvement in technical facilities [3].
Silent glue ear together with narrow ear canals would make the examination of tympanic membrane difficult, and OME can easily be neglected to a superficial examination [6]. When inadequately treated or left untreated, OME may lead to delayed sequelae and complications like acute otitis media with tympanic perforation, retraction pockets, tympanosclerosis, adhesive otitis media, cholesteatoma all clinical conditions characterized in children by permanent hearing loss and impairment in development of speech and language [7]. It is often associated with an abnormal or malfunctioning ET, which causes negative pressure in the middle ear and leaking of fluid from tiny blood vessel or capillaries into the middle ear. Problems with the ET can be caused by viral infections, injury or birth defects (such as cleft palate) [8]. Hypertrophy of the adenoids and ET dysfunction are often considered to be causal factors of OME. About 25-30% of children with O.M.E. have no significant medical history and the disease could be identified only through regular screening. The remaining approximately 70%, have more or less vague symptoms such as episodes of earache and conductive hearing loss detected by parents, they rarely show abnormal behaviour or scholastic deterioration detected by teacher and educator [9]. Because protracted hearing loss in young children may delay or permanently change their communication skills and may lead to behavioural and educational difficulties, clinicians and others are concerned about the possible role of OME on these outcomes. More recently, atopy and specific gene abnormalities [10,11] have also been implicated as host risk factors for OME.
We performed this study to determine the epidemiology, clinicoaudiological profile like the characteristics of the presenting symptoms, the otoscopic findings, the severity of the hearing impairment and radiological characteristics as well as treatment outcome of children less than 12 years old who suffered from Otitis Media with Effusion (OME) including the intraoperative findings and to assess the effect of four different surgical treatments for glue ear (Myringotomy with grommet insertion, Myringotomy with Grommet plus adenotonsillectomy, Myringotomy with grommet plus adenoidectomy alone, Myringotomy with grommet plus tonsillectomy alone), on improvement in hearing and, assuming one or more treatments to be effective, to identify the appropriate indications for surgery.
Materials and MethodsThe study was conducted from January 2011 to January 2015 in Sur Ministry of Health Hospital and was performed upon 150 children up to 12 years old who were diagnosed as OME and who were coming from different areas in South Sharqiya Governorate. The study was approved by Ethical commitee, Sur Hospital and an informed consent was taken from the parents of the concerned children. Patient’s demographic data included age, sex and presenting symptoms (hearing impairment; ear block; scholastic retardation and poor performance at school; snoring and/or mouth breathing; otalgia; tinnitus); all the patients underwent ENT examination, including pneumatic otoscopy and otomicroscopic evaluation. If present the wax was carefully removed with cerumen hook or irrigated with saline at room temperature. Children with mental disability, with history of cleft lip or cleft palate repair procedures, acute otitis media and patient with tympanic membrane perforation were excluded from the study. The character of the tympanic membrane was determined as appearance (whether normal, dull or retracted), presence of fluid in the middle ear as air bubbles or fluid level and the colour of the tympanic membrane (yellow, grey, blue or amber). All patients underwent tympanometry using the middle ear analyzer model GSI 33 version 2.0 serial A 1354 (Garson-Stadler Inc., USA); the results were evaluated according to Fiellau-Nikolajsen's modification of Jerger's system.
The results were classified as Type A (+100 and -100 daPa), Type B (no pressure peak), Type C1 (-101 and - 200 daPa), Type C2 (-201 and -300 daPa). Furthermore a Pure Tone Audiometry (PTA) was used to assess the hearing threshold in children. The PTA was done using six frequencies (250, 500, 1000, 2000, 4000, 8000 Hz). The degree of hearing impairment on Audiometry was recorded as follows; (1) mild hearing loss: 25 to 44 dB HL, 2) moderate hearing loss: 45 to 64 dB HL, 3) severe hearing loss: 65 to 80 dB HL and 4) profound hearing loss: more than 80 dB HL. Further investigation, if indicated, included plane x-ray of the neck in lateral views to assess adenoid size, were measured by Adenoid/ Nasopharyngeal ratio i.e. A/N ratio, where N is the distance between the posterior superior edge of the hard palate and the anteroinferior edge of the sphenobasioccipital synchondrosis, and A is the distance between the maximum convexity of the adenoid and a line drawn along basocciput. A/N ratio below 25% was scored as 1+, those between 26% and 50% as 2+, those between 51% and 75% as 3+, and those between 76% and 100% as 4+.
OME patients were treated with medical therapy consisting of local nasal steroid, systemic and/or local decongestant and in presence of Upper Respiratory Tracts Infections (URTI) or adenoid inflammation systemic antibiotics were administered. After two weeks the children underwent new examination that confirmed the treatment up to 12 weeks or with evidence of lack of medical therapy benefit lead to surgical choose in form of Myringotomy alone or may be adenotonsillectomy. The clinical course was followed up to six months after surgery.
ResultsThe total number of patients with OME was one hundred and fifty, 91 boys (57.6%) and 59 girls (37.3%); The age of children ranged from 2 to 12 years old with a mean age of 7 years (Standard deviation- 2.970). Table 1 shows the distribution of the cases according to age and sex.There was a peak incidence between males and females at 8 years of age wherein n=20, but the Chi Square test was not statistically significant with calculated P value was at 0.848 which is more than statistically significant value of 0.05.
Regarding the presenting symptoms, 51.9 % of the children had hearing impairment (n=82), closely followed by complaints made by teachers regarding scholastic retardation and inattentiveness at school with poor performance at school grades that has worried many parents (n= 26) constituting 16.5% of the symptoms. Snoring and mouth breathing also was mostly complained by parents (n= 22) forming 13.9% of the presenting symptom, Otalgia (n=6), tinnitus (n=6) were rare presentations, and 5 cases were detected incidentally during routine ENT examination. Table 2 showed the distribution of presenting symptoms in order of frequency.
As for otoscopy the retraction of Tympanic Membrane (TM) was the commonest sign (n= 61 i.e. 38.6%) followed by hyperaemia of TM (23.4%), dull TM (32, air bubbles behind the TM (7.6%) and fluid behind TM (5.1%), (Table 3).
Tympanometry (Table 4) evidenced a type B curve in 78.5% of (124 cases ), type C1 in 8.2% (n=13) and type C2 in 7.6% (12 cases), while hearing threshold performed on the children aged more than 5 years old, corresponding to 62 cases.
Pure tone audiometry (Table 5) showed mild hearing impairment in majority of the OME cases n=92 i.e 58.2% followed by Moderate hearing loss ranging from 45 to 64 Db n=48 and formed 30.4% , only n=10 cases had profound hearing loss more than 80 Db 6.3%
Statistical correlation between age (as dependant variable) and PTA+ Tympanometry.
(@)- R Squared = .042 (Adjusted R Squared = -.005)
The relationship between the type of tympanogram and the hearing threshold (Table 6) showed that 74(55.4%) patients with type B tymapnogram had Mild hearing loss on PTA ranging from 25 to 44dB HL and 40 cases (28.9%) OME cases with type B tracing had moderate Hearing loss ranging from 45 to 64Dbhl, Chi square test was statistically significant between hearing threshold and corresponding tympanogram with P value was less than 0.01.
Regarding the size of adenoid (Table 7) based on a A\N ratio, 34 patients presented a grade 1+ (12.2%), 35 cases (20%) grade 2+, 42 patients (43.3%) had grade 3+, and in 39 cases (24.5%) the adenoids resulted of grade 4+. It was evidenced a strong correlation between the adenoid size and the tympanogram; in fact the 35 cases (25.3%) and 29 cases (23.5%) of children with adenoids grade 3+ and grade 4+ presented a type B tympanogram respectively.
The relationship between tympanometry and adenoid size shows that 35 cases with type B tracing had a grade 3 adenoid and these relationship yielded a statistically significant P Value of less than 0.05 (Table 8).
Medical line of treatment (Table 9) was tried initially as per the table depicted, but these patients did not have the expected relief with only medical treatment and surgical option had to be undertaken. Surgical treatment was the modality of management in these 150 patients. 60 cases underwent Myringotomy with grommet and adenoidectomy alone 29.2%.35 cases had Myringotomy with grommet and adenotonsillectomy, 51 cases had tonsillectomy alone along with Myringotomy and grommet insertion.
The above table (Table 9) shows that majority of the males and females (n=49 and 27 respectively) received nasal steroid sprays and P value as per Pearson Chi square test was statistically significant (P value was less than 0.05).
Major number of males and females (n=32 and 28 respectively) underwent Myringotomy with grommet including adenoidectomy alone and these sex variations plotted against different surgical modalities were statistically significant in our study with P value less than 0.05 (Table 10).
The mean Air bone gap was 23.9 ± 6.33 dB in patients who underwent Myringotomy with gommet and Tonsillectomy alone closely followed by Myringotomy with grommet and adenotonsillectomy group of patients with mean Air bone gap of 22.2 ± 6.07 Db (Table 12). The cases were followed up post surgery at 6 weeks, 3 months and 6 months and the following table demonstrates that there has been significant improvement in the mean air bone gap over a period of time with improved hearing. The findings were statistically significant with P value of less than 0.05(Table XII).
DiscussionOtitis media with effusion is a very common paediatric disease characterized by chronic accumulation of fluid within the middle ear, and occasionally in the mastoid air cell system without signs of acute infection. The time that the fluid has to be present for the condition to be chronic is generally around 12 weeks [12]. The incidence decreases with increasing age i.e. from 40% at two years to 1.4% at 11 years. The study demonstrated that OME in South Sharqiya province is slightly more among boys (n= 91, i.e. 57.6%) than girls (n= 59, i.e., 37.3%); this is comparable with some studies which demonstrate that males have a significantly higher proportion of OME (P=0.0067) [13]. The finding that OME is more common among males than females is consistent with the maleto-female ratio found in other international studies [14]. In the review article of Zeilhius, et al. [15], he found that the prevalence of OME is bimodal the first peak at 2 years and the second peak at 5 years of age. In the study of the median age group was found to be 7 years. Environmental factors such as pollution and recurrent upper respiratory tract infections are usually associated with high incidence. Seasonal relationships are confirmed with a peak in winter [16]. The most frequent presenting symptom is mild to moderate conductive hearing loss. Attacks of episodes of otalgia often coincide with an upper respiratory infection which may sometimes be recurrent. Hearing loss often fluctuates in severity. Often children with O.M.E. increase the sound of radio and T.V. to compensate their hearing, disturbing the others. They may become lazy, dreamy, and nervous. Their speech, language and cognitive functions may be affected. They may show deterioration in their school, because they cannot follow the teacher [17].In Syed, et al. [18] the common presenting symptom was fullness in the ear (50.3%) [18]. I n our study it was just around 1.9%.Some children may complain of ear fullness or ear block. Tinnitus is another symptom that children described infrequently most probably due to Eustachian tube dysfunction. (Our study 3.8%). In our study most of the patients presented with hearing impairment 51.9 %, followed by poor performance at school 16.7%.A general ear examination may show dullness, air bubbles and fluid behind the tympanic membrane or reduced mobility. In Syed et al. the common sign seen by otoscopic examination was dull eardrum (72.18%) [18], while in our study the commonest was retraction of tympanic membrane (38.6%).
OME was diagnosed by history, otoscopic finding, conductive hearing loss on PTA or play Audiometry and impedance tympanogram. The degree of retraction of the pars tensa may be assessed by shortening of malleus handle, retraction pocket at pars tensa, atrophic transparent tympanic membrane. The degree of retraction of the tympanic membrane reflects the negative middle ear pressure which reduces the mobility of the membrane. The colour and loss of translucency of the membrane range from pale grey or amber to a black or so-called ‘blue drum’ [19]. It may be thickened, dull and opalescent or thin and reflective. Fluid levels and air bubbles may be visible within the middle ear cleft. Atelectatic change of the pars tensa and pars flaccida may be present to a variable degree. Pure tone audiometry provides some assessment of the severity of the disease. It can be used as a guide by which to monitor the progress and the effects of treatment. Tympanometry provides an effective screening test for the detection of negative middle ear pressure although it will not distinguish between such a pressure change with and without middle ear effusion. The type of fluid found in the middle ear during Myringotomy in cases of OME varied from a thick mucus “glue-like” secretion to thin serous fluid. Analysis of the constituents of the effusion showed that the viscosity is correlated with the concentration of mucin [20]. Not all patients diagnosed clinically as having OME were found to have fluid present in the middle ear at Myringotomy. It is still avidly debated in the literature whether this common occurrence is due to exposure to nitrous oxide during general anaesthesia [21].
The most common type of tympanometry results seen among children with OME in our study was type B (n=124,78.5%), Kemaloğlu, et al. [22] and Pan, et al. [23] reported that B-type tympanogram positive predictive values were 96% and 92.57% respectively. Type B tympanogram is the best diagnostic tool for predicting OME in the children with parental suspicion of hearing loss .Type A or C tympanogram sometime could be seen in the group of children with OME, especially peak pressure value is less than–300 daPa. The mean Air bone gap obtained from PTA was 23.9± 6.33 dB. Meanwhile, most cases showed mild degree of hearing loss (n=92, 58.2%). Thompson in 2008, Martines et al. in 2010 and 2011 revealed that the worse conductive hearing loss among children with OME was of moderate degree, which constitutes up to 10% compared with 20- 35% having mild degree hearing loss [24]. These results suggests that the degree of conductive hearing loss among cases with OME cannot be worse than a moderate hearing loss as the skull vibrate at intensities greater than 60-70 dB hearing level allowing the signal to go straight to the inner ear; anything greater than this is considered to be mixed hearing loss [24].
The study was able to demonstrate a high prevalence of adenoid size especially grade 3+ (43.4%) among patients with OME, this was consistent with another recent study done in Nigeria in 2010 on number of children with OME, where they found a significant association between type B tympanogram and the presence of significant nasopharyngeal obstruction with odds ratio of 4.4 [25]. It was possible that such adenoid, even though of small size, encroached laterally to obstruct the ET of the involved ear, such lateral encroachment was reported to be significant in influencing development of OME. It was also possible that other risk factors for OME such as ET dysfunction were probably responsible for the development of OME in those children with small sized adenoids [26]. While most cases of OME will resolve spontaneously, some children will need intervention because of the effects of hearing loss.
Generally surgical treatment is indicated where conservative treatment failed to work, in long standing disease (chronic), in cases of recurrent attacks of OME or when the affect of hearing loss on the child is severe. Different forms of surgical treatment are available. These include Myringotomy, adenoidectomy, adenotonsillectomy, insertion of ventilation tube, or a combination of all [27]. Myringotomy alone has been proven to be of minimal therapeutic benefit as the incision area will close very soon postoperatively [28]. Around 38% of patients in our study underwent Myringotomy with grommet and Adenoidectomy alone, and 32.3% of cases underwent Myringotomy with grommets and tonsillectomy as well. The efficacy of adenotonsillectomy on OME has been demonstrated by several randomized and controlled studies. It was speculated that tonsil and adenoid may play a role as an infectious focus to OME, so that some authors stated that, patients suffering from recurrent or chronic OME may benefit from adenotonsillectomy due to removal of an infectious source in the nasopharynx rather than the removal of a large adenoid mass [29].
ConclusionIn conclusion, Middle Ear Effusion is a very common childhood disease, affecting the child's hearing at the most critical age (2 years), the Child's speech and language development and its education. Hence the problem has to be treated with special consideration. Early detection through screening programs and health education followed by immediate proper treatment are the best known effective measures to fight this disease. Among the treatment options adenoidectomy and Myringotomy with grommet insertion had shown a better improvement in hearing followed by adenotonsillectomy and Myringotomy with grommet insertion . It is recommended that surgical intervention should be attempted as early as possible when the medical management fails to respond. Among the various surgical interventions adenoidectomy was found to have a better improvement in hearing in our study with better hearing outcome.
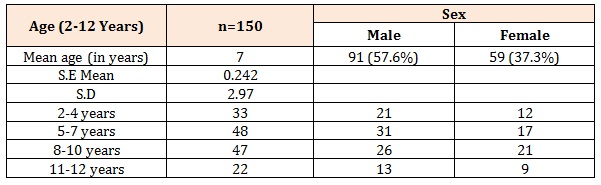
Table 1: Statistical correlation between age and sex in patients with OME.
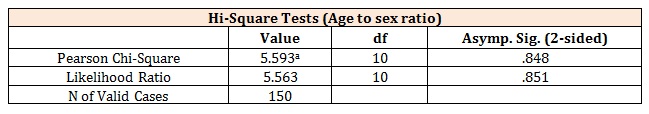
Table 2: Symptom complex with which the OME patients presented.
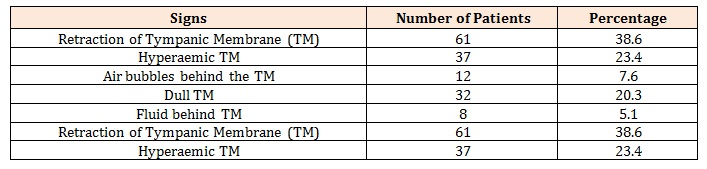
Table 3: Tympanic membrane signs with which OME patients presented.
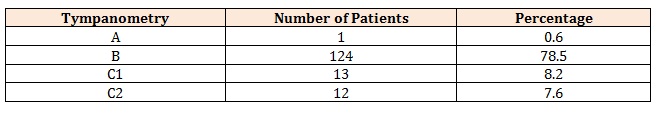
Table 4: Tympanometry results in patients with OME.
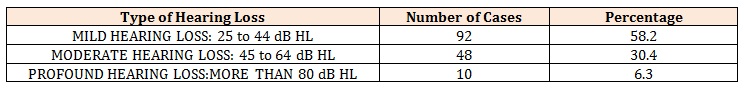
Table 5: PTA findings as recorded in OME patients.
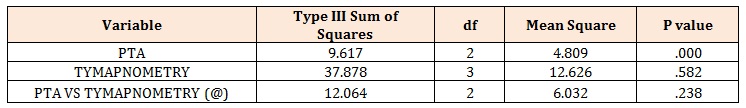
(@)- R Squared = .042 (Adjusted R Squared = -.005)
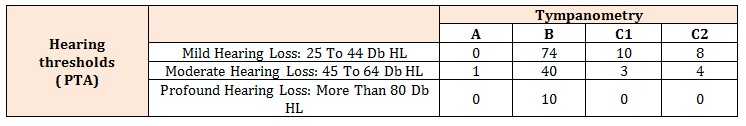
Table 6: Correlation between PTA and tympanometry.
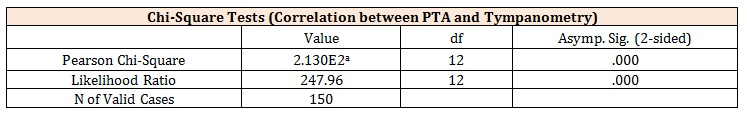
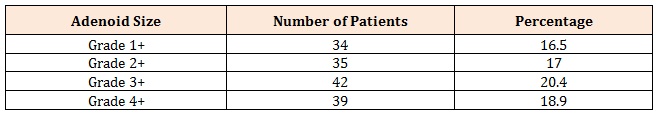
Table 7: Adenoid size among OME patients.
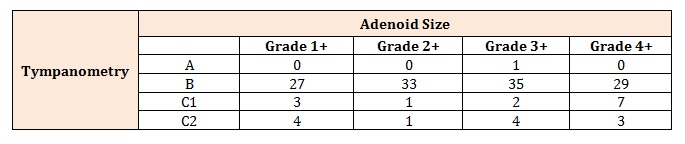
Table 8: Relationship between tympanometry and adenoid size among OME patients.
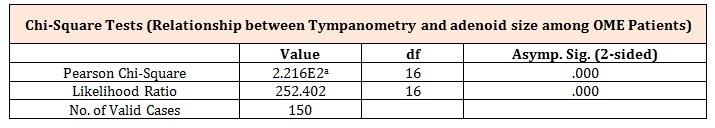
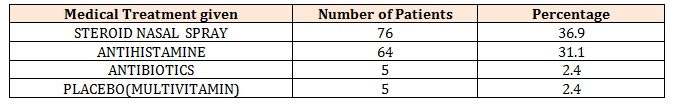
Table 9: Medical line of management initiated for OME patients under Study.
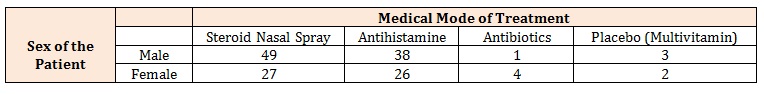
Correlation between the medical line of treatment and sex of the patient with OME.
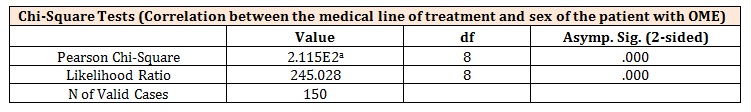
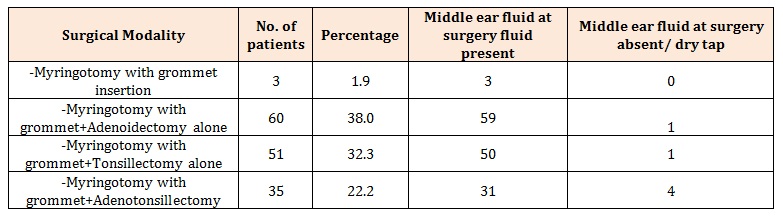
Table 10: Various Surgical mode of management that the OME patients underwent.
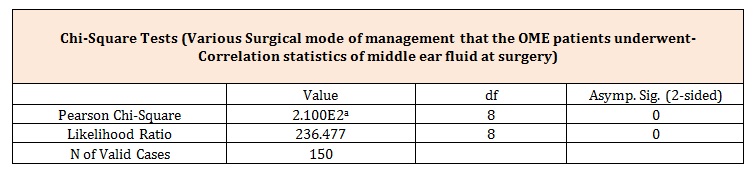
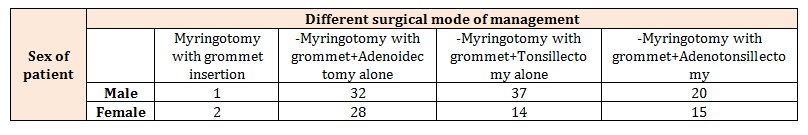
Table 11: Correlation between sex of the patient with OME and different surgical modalities of management instituted.
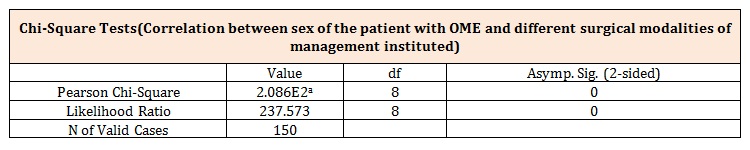
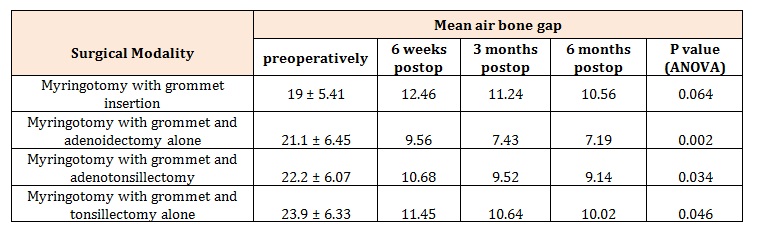
Table 12: Comparison of pure tone audiometry readings before and after various interventions among the study population.
Chat with us on WhatsApp