Citation: McDowell C, et al. Reducing Rumination of a Child with Autism Spectrum Disorder Using Post-Meal Tooth Brushing. Psychol Pshycholgy Res Int J 2017, 2(3): 000126.
*Corresponding author: Claire McDowell, Rm G101,School of Psychology, Ulster University, Coleraine Northern Ireland, Tel: 02870123086; Email: ce.mcdowell@ulster.ac.uk
Background: Rumination is defined as the regurgitation, chewing and re-swallowing of partially digested food. It is estimated that it occurs in about 10% of individuals with developmental disabilities.
Method: An AB design was employed to assess the effectiveness of an intervention designed to reduce the number of occurrences where rumination followed eating in two settings, one of which acted as a control setting
Materials: Materials included a digital wristwatch, pen and paper based food diary and a child sized manual toothbrush and mint flavoured children’s toothpaste.
Results: Baseline measures showed that the percentage of sessions where rumination occurred was similar in both the snack and lunch settings. The intervention which was implemented in the snack setting only resulted in a decrease in the number of times rumination occurred after school snack time. There was no significant decrease in rumination following lunch which remained under baseline conditions.
Conclusions: The data add to the PBS literature on non-aversive interventions for rumination and suggest a healthy, age appropriate and functional means of decreasing the behaviour in a young child with Autism Spectrum Disorder
Keywords: Rumination; Tooth brushing; ASD
Research has demonstrated that meal time and feeding disorders occur frequently in children with Autism Spectrum Disorder (ASD) [1], and can include food refusal, food selectivity, food packing and rumination [2,3]. Rumination is defined as the regurgitation, chewing and re-swallowing of partially digested food [4-6] and it is estimated that rumination occurs in about 10% of individuals with developmental disabilities [7]. The long term physical effects of rumination include malnutrition, esophagi is, and dehydration and reduced resistance to disease [8]. Other side effects may include tooth decay, halitosis and social exclusion due to malodorous breath. In some cases, rumination may be caused by a medical condition such as gastrointestinal problems. However, when no medical reasoning can be found functional analysis is often conducted to examine the environmental factors responsible for rumination [9-11]. Some interventions to reduce rumination have focused on providing aversive or punitive consequences contingent on the behavior. The aversive stimuli range from electric shocks to lemon juice or alternative strong flavors presented into the mouth [12-15]. More recently, Dominguez, Wilder, Cheung, and Rey (2014) successfully reduced rumination of an 11-year-old boy with ASD using a verbal reprimand [16]. They suggest that while some studies report effective treatment based on non-aversive interventions such as satiation, differential reinforcement schedules, extinction, special feeding techniques, and contingent exercise, often these interventions are only effective for some, and require special planning, preparation and additional resources [17,18].
Positive behavioral support (PBS) has been defined as practice based on the assessment of the broad social and physical context in which the behavior occurs [19]. Person-centered values are considered a foundation in the development of PBS, with Carr, Dumlap, Horner, Koegel et al. (2002) describing the evaluation procedure of PBS as incorporating a technological criterion as well as values criterion [20]. These criteria include considering the intrusiveness or level of restriction of the treatment, and the social acceptability of the treatment. Nonrestrictive, non-intrusive based procedures that have effectively reduced rumination include satiation procedures that include the provision of a satiety level of food post meal times, through; providing larger portions at meal times [21-23] providing supplemental food up to 30 minutes after mealtime or higher ratios of certain food types such as starches, [25-27] or fruit and vegetables thus increasing the stimulation sensation the meal provides. Although food based treatments are effective, easy to implement and more socially acceptable than punishment based treatments, limitations of this type of intervention can include weight gain [28].
Rhine and Tarbox (2009) provided post-meal chewing gum to child with ASD. A 3-month follow up showed that chewing gum reduced levels of rumination and they remained low. Wilder et al. (2009) reduced rumination by delivering a preferred food flavored spray on a fixed-time delivery. The authors of these studies argued that this type of intervention may be successful as sprays or chewing gum may provide similar reinforcing effects and rumination, or reduce or alter the reinforcing effects of rumination in some way. In addition, they are potentially less harmful than satiation based interventions because they are calorie free. The current case study aimed to extend this work by using post meal tooth brushing rather than flavored spray or gum chewing after meals. Tooth brushing was deemed not only to be an age appropriate skill that was already part of the child’s independent skill repertoire, but to also have additional positive benefits in encouraging good oral hygiene [10,29].
MethodAn AB design was employed and the study focused on two naturally occurring settings in school, morning snack and lunch time, with lunch acting as a control setting. The target behavior was operationally defined as the return of pre-chewed food into the mouth indicated by; a stretched neck, a gurgling sound, the swelling of cheeks and a swirling sound. Rumination ended after the sound of a loud swallow and the child had the ability to carry out an oral task without regurgitated stomach contents escaping the mouth. Whether or not rumination occurred was recorded beginning immediately after the child indicated she had finished eating. A session was defined as the hour period immediately following either snack or lunch. The percentage of sessions where rumination occurred was calculated by dividing the number of sessions where rumination was observed to occur, by the total number of sessions in each of the settings.
ParticipantThe participant was a 6 year-old girl who had a diagnosis of Isodicentric 15 (Idic 15); a chromosomal disorder characterized by a duplication of Chromosome 15. The participant had also been given a diagnosis of ASD, which is frequently reported in individuals with Idic. 15. She attended a Special Needs Educational School, where the second author worked as her classroom assistant, and had displayed the ruminative behavior for approximately three years. Testing had ruled out a medical cause for the ruminative behavior including any problems with reflux or the esophageal area. A previous intervention for rumination based on the principle of satiation and increasing the amount of protein consumed had been unsuccessful.
Materials and SettingObservation and recording of the occurrence of rumination occurred in 2 settings during the school day. The settings consisted of snack time in the classroom (10.00-10.30am), and lunch time (12.15-12.45pm) in a communal dining hall. In both settings, the child had access to the usual eating implements and vessels and was free to choose foods from a range that were available to all children at these times. Using pen and paper, the second author also recorded the food choices and what was eaten by the child during all snacks and meals. The second author used her digital wristwatch to time the hourly observation period following each meal. A child’s manual toothbrush and mint flavored fluoride toothpaste were used for the tooth brushing intervention.
ProcedureBaseline During baseline, food was presented to the participant in a typical way. During school snack time, a ‘cafe’ situation is set up in the class room. The participant typically used speech and/or an augmentative communication system (PECS; Picture Exchange Communication System) to request her food, which was placed on her plate, before she returned to a snack table to sit with her classmates and the second author, to eat. At lunch time the participant ate in the dining hall with the rest of her class. She requested food from the selection available using speech or PECS. Food items were placed on her plate and she took them to a table to sit with the rest of her class and the second author. When the participant either finished her meal, or that she had finished eating, the plate was returned to a serving hatch and the child returned to her classroom under the supervision of the second author who recorded whether or not rumination occurred in the 1-hour period that followed.
Intervention Following 11 sessions under baseline conditions, the post meal tooth brushing intervention was implemented in the snack time setting for 37 sessions, while lunch time remained under baseline conditions for a further 37 sessions. Immediately upon completion of the snack, the child and second author walked to a bathroom area off her classroom and asked to brush her teeth using a manual tooth brush and mint flavored toothpaste. The first author used a wrist watch to time 2 minutes of tooth brushing. Verbal prompts and praise were used to encourage the child to complete the activity. Following lunch in the dining hall, the child returned to her classroom as normal.
ResultsBaseline measures of the number of sessions where rumination occurred were taken for 11 sessions and in the snack setting and 48 sessions in the lunch setting. Baseline data from the food diary suggested that rumination was more likely to occur following a meal if the child had eaten sweet food items. Figure 1 shows that the percentage of snack time sessions where rumination occurred was 64%. The percentage of sessions where rumination occurred in the lunch time setting was also 64%.
The intervention was implemented in the snack time setting over a further 37 sessions while baseline data continued to be gathered in the lunchtime setting. Figure 1 shows that rumination occurred in 35% of snack time sessions under the intervention condition, while 59% of lunchtime sessions resulted in rumination. Using the percentage reduction measure (PRM) also known as the mean baseline reduction statistic (MBLR) to calculate the mean percent reduction in behavior, the mean of treatment observations was subtracted from the mean of baseline observations for behavior in both settings. Results show a 45.3% reduction in rumination in the snack condition, compared to a 7.8% reduction in the lunch setting where no intervention occurred [30-32].
DiscussionBaseline data, including a food diary, indicated that rumination was more likely to occur when preferred sweet foods were ingested. This suggested that the potential reinforce was the flavor of regurgitated food. Post-meal tooth brushing was employed to reduce the behavior as it was hypothesized that removal of the preferred flavor would decrease the motivation to ruminate. The results of the current case study indicate that tooth brushing effectively reduced ruminative behavior by 45% in the setting where it was implemented. Rumination did not decrease in the control setting where tooth brushing did not follow eating. The food diary showed that there were no observable changes in relation to the types of foods available during snack and lunchtime before or after intervention. There were also no observable changes in the types of foods chosen by the child before or after intervention. Therefore, it is unlikely the decrease in rumination in the snack setting was simply due to less sweet food types being available or being consumed.
Although only based on results from one participant, these findings add to the research on the use of non – intrusive or restrictive practice interventions to reduce ruminative behavior following meals. However, as with the findings of Wilder et al. (2009), it is not clear if the intervention worked by competing with rumination in terms of the motor responses required (differential reinforcement of incompatible behavior) or by reducing the motivation to ruminate by removing the flavor of recently ingested foods. It is worth noting that if removal of the flavor of recently ingested food was a variable, then preferred flavors will vary across individuals, hence the importance of a food diary as part of similar interventions. While future research should of course seek to replicate similar interventions with a larger number of participants, nonetheless, the current study has successfully addressed the concern of ruminative behavior in a young child by reducing the behavior in a way that does not negatively affect her health. It also promoted dental health by keeping the mouth clean and so lessening the physical and social side effects associated with rumination. As a result, post meal tooth brushing has been implemented as a normal part of her daily school and home routine.
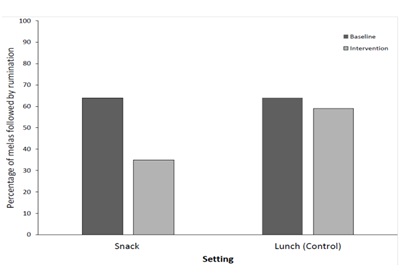
Figure 1: Percentage of meals where rumination followed eating in both settings, before and after the introduction of post meal tooth brushing in the snack setting only.
Chat with us on WhatsApp