
Citation: Abuelenain DA, et al. Polymerization Shrinkage Stresses of Low Shrink Versus Conventional Micro-Hybrid Composites MOD Restorations: A 3-D Finite Element Analysis Study. J Dental Sci 2016, 1(2): 000110.
*Corresponding author: Dalia A Abuelenain, Division of Biomaterials, Restorative Dentistry Department, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia, PO Box: 14785, Zip Code: 21343, Email: dabualenain@kau.edu.sa, daenain@gmail.com
Using 3-D finite element analysis (FEA), this study aimed to test the hypothesis that dimethacrylate-based composites (Filtek Z250) with greater polymerization shrinkage will show higher stress generation, within the restorative material system and the supporting structures, than low shrink silorane-based composites (Filtek P90), particularly in large cavities (MOD). A tooth model for maxillary first molar with a MOD cavity was constructed using Solid works Premium 2012 software. The ANSYS 13.0 software was used to assign the materials and tissues properties. A 3D structural static finite element analysis was then conducted. Data analysis revealed that the resulting Von Mises Equivalent Stresses (MES) generated within the enamel, dentin and composite were higher with Filtek Z250. MES increased monotonically as the polymerization process progressed. The highest MES existed at the axio-gingival line angle and cervical cavo-surface margin of enamel, dentin and adhesives. Within the composite material, the highest MES existed at the restoration occluso-axial surface. As a clinical consequence, the composite material system with higher polymerization shrinkage stresses is more susceptible to microcracking and accordingly earlier failure than low shrink system.
Keywords: Finite element analysis; Flexure strength; Low shrink composite; MOD restorations; Von Mises equivalent stress
Upon polymerization of the conventional dimethacrylate monomer, the single methacrylate molecules move towards each other and linked to form a polymer network. Monomer molecules are at a distance of 3-4 Aº when they polymerize the distance between the polymers units are reduced to 1.5 Aº. This produce polymerization shrinkage of 1.5-5% [1]. Together with this shrinkage, stresses that challenge the integrity of the tooth/restoration interface are always produced [2]. When the polymerization shrinkage stress encompasses the bond strength of the adhesive, used to bond the composite to tooth structure, a microgap will be produced at the tooth/restoration interface with subsequent marginal leakage, pain, sensitivity and secondary caries. If the adhesive bond strength, however, exceeds the polymerization shrinkage stresses, a cuspal deflection, postoperative hypersensitivity or enamel fracture may, however, occur [3,4]. Silorane monomers have been introduced to the dental market as low shrink alternative to dimethacrylate monomers [5,6]. Upon polymerization, the silorane rings opened, flattened and extend towards each other to form the polymer network [7]. The ring opening partially compensates the shrinkage resulting from molecular bonding; the resultant volumetric shrinkage (<1.0%) is comparably lower than the conventional dimethacrylate-based composites [8,9]. Reduced micro leakage [10,11] and tooth deflection [12] would be therefore expected with silorane-based composites. In addition to the type of resin monomer, some other factors could affect the magnitude of polymerization shrinkage/stresses. They include; reaction rate, [13,14] the property of resin composite (e.g. stiffness and Poisson’s ratio) [7,15] adhesive stiffness, [16] cavity geometry, [17] and tooth structure stiffness [18]. For instance, rigid composites increased tooth stiffness and hence reduced deformation regardless of the higher polymerization shrinkage stresses [19]. There is currently no theoretical evidence to support the hypothesis that dimethacrylate-based composites with greater polymerization shrinkage will have stress generation, within restoration complex and supporting structure, than low shrink silorane-based composites. This particularly applies to large cavities as MOD in maxillary first molars where the combination of diverse materials and complex geometry of large cavities makes the stress distribution analysis complicated. Accurate analysis of the stresses generated within MOD toothrestoration system is therefore required to compare low shrink silorane-based versus dimethacrylate-based composites.
In recent years, there has an increasing interest in the biomechanical behaviour of biomaterials and human tissues that provide an answer to most questions in the dental field. The dental research, however, is costly, timeconsuming and may be ethically questionable. The use of in vitro simulation and numerical models has been recognized as a valuable tool for saving money and time associated with laboratory and clinical research. The finite element analysis (FEA) is a computer-based numerical technique with which a structure is disassembled into its component parts; the stress and deflection of each component can then be assessed. The FEA has proved its capability for the deformationstress analysis in a wide range of applications relevant to almost all dental disciplines [16,19,20]. It provides an accurate analysis of stress distribution and displacement all over a structure under any type of static or cyclic loading [21]. Idealizations should be as close as possible to real situations particularly in dental applications e.g., threedimensional modelling, actual cyclic biting forces and material behaviour. The aim of the present study was, therefore, to analyze and compare the stresses generated within the restoration-tooth system in MOD restorations using low shrink Filtek P90 and the conventional Filtek Z250 with their respective adhesives using 3D FEA. To achieve this goal, the stress-strain behaviour of both composites and their associated low shrink P90 adhesive and single bond universal adhesive has been firstly characterized using three-point bending test.
Materials and MethodsAll materials used in the study are products of 3 M ESPE (St, Paul, MN, USA) and the materials are listed in (Table 1) with technical details.
Three-point Bending TestRectangular specimens (n=10) for each material were prepared using a split Teflon mold of 25×2×2 mm3 according to ISO specification no. 4049 [22]. Celluloid strips covered with microscopic glass slides were placed at the top and bottom of each specimen to reduce inhibition of polymerization caused by oxygen and to provide smooth surfaces. They further ensured removal of excess materials and consistent packing of samples. Each specimen was light-cured using a conventional Quartz Tungsten Halogen curing device QTH (LITEX 682 Dentamirica, USA) with 7 mm curing tip. The light was applied over 4 overlapping increments of 20s each; that was done from both sides of the mold. The intensity of the light source was 700 mW/cm2; it was verified between samples using a radiometer (LITEX 682 Dentamirica, USA). Specimens were removed after curing and the excess material was carefully removed using a sharp scalpel blade. Samples were stored in dark dry containers for 7 days before testing. Flexure strength of each material was determined using a three-point bending test with a universal testing machine (Instron 5944, USA) at a crosshead speed of 0.25 mm/min and 2 N loading cell. Prior to testing, the dimensions of each specimen were measured using a micrometer. The flexural strength, modulus, yield strength and fracture strain were calculated using Blue hill 3 software. The obtained data were statistically analyzed at 0.05 level using one-way ANOVA and then paired-t-test to compare between any two groups. The statistical analysis was carried out using the SPSS system for Windows (SPSS 16.0).
3-D Finite Element Analysis (FEA)The profile of an extracted sound human first maxillary molar was carried out using a cone beam CT in a form of an STP image formatted file (Figure 1A). The 3-D geometrical idealization of first molar with its supporting tissues was constructed using Solid Works Premium 2012 software (SP0.0X64, Dassault Systémes Solid Works Corporation, Waltham, MA USA) (Figure 1B). The anatomic details of the natural tooth were reproduced with a scale 1:1 [16]. The thickness of the periodontal ligament was assumed 0.25 mm and that of the cortical bone was 2 mm. The bone with the surrounding soft tissue extended for 14 mm along the mesio-distal direction; the bucco-palatal width of bone was assumed 11 mm [23,24]. A cavity for MOD restoration was prepared with the geometry and dimensions shown in (Figure 1C).
The adhesive was, then, applied with a thickness of 45 µm, which is the smallest thickness that can be simulated in FEA. A resin composite was then used to fill the cavity and restore the original occlusal and proximal surfaces. The different parts of analyzed MOD restored tooth assembly are presented in (Figure 2A and B). The SolidWorks uses different file formats that can be exported to ANSYS 13.0 software (ANSYS Inc., Canonsburg, PA, USA). The IGES file format was invoked in the present work to export the geometries to the simulation software. ANSYS 13.0 software was employed to import the constructed tooth model. The mesial, distal and apical borders of the model were fixed with no separation allowed at the contact surfaces of the parts of the assembly. The software generated a computational mesh; mesh trials were first performed for the convergence of the total elastic strain energy to achieve the final analyzed model shown in (Figure 2C). The number of the nodal points and tetrahedral elements of the zones of the model are listed in (Table 2). The mucosa and the periodontal ligament were considered as a continuous body as in reality. The materials of the model zones of the tooth were assumed to be isotropic homogenous and linearly elastic.
Due to the plastic deformation behavior observed for the analyzed composites and adhesives, the volumetric shrinkage was applied in increments to ensure incremental convergence of the results. An equivalent decrease in temperature of the analyzed composite corresponding to an assumed coefficient of thermal expansion simulated its behavior due to shrinkage. A 3-D FEA was carried out on the model of the restored tooth to have the corresponding fields of the generated von Mises equivalent stress (MES). This detected the site of the highest MES value within each part of the model.
ResultsFigure 3 presents the mean stress-strain curve of the two composite systems and their associated adhesives. The flexure strength and modulus of Filtek Z250 (188±12 MPa and 23±2 GPa respectively) were significantly (p <0.05) higher than the corresponding values (146±23 MPa and 17±2 GPa respectively) of Filtek P90 low shrink composite. However, there was no significant difference (p=1) observed between the two composites regarding their fracture strain. The flexure strength and modulus of Single bond universal adhesive (22±7 MPa and 0.6±0.1 GPa) however were significantly (p=0.0001) lower than those of P90 system adhesive (79±21 MPa and 2±0.6 GPa). Like composites, there was no significant difference (p=0.8) observed in the fracture strain between Single bond universal adhesive and P90 system adhesive. The polymerization shrinkage [25,26] as well as the Poisson’s ratio [27,28] of the tested composites and adhesives were obtained from the literature. Due to the small thickness of the adhesives used in this study, their polymerization shrinkage values were not considered. The elastic modulus [29-31] and Poisson’s ratio [27,28] of the periodontal ligament, cancellous bone, cortical bone, and mucosa were also obtained from the literature.
3-D Finite Element Analysis (FEA)Figure 4 presents the development of highest MES value within the four crown regions of the analyzed restored tooth during the polymerization shrinkage of the two composite systems used in the present study. The stresses generated within the enamel, dentin and composite were invariably higher with hybrid Filtek Z250 (654, 113 and 146 MPa respectively) than with Filtek P90 (503, 80 and 80 MPa respectively). However, there was no difference between the generated stresses within the adhesive layer on using both composites with their corresponding adhesive.
As expected the value of the highest MES increased monotonically as the polymerization process progresses. (Figure 5) shows the sites of the highest MES value generated within the four zones of the crown of the idealized restored molar due to composite polymerization shrinkage. Such sites revealed no difference between using low shrink Filtek P90 composite and microhybrid Filtek Z250 composite. The highest MES values existed at the axio-gingival line angle and cervical cavo-surface margin of the enamel, dentin and adhesive zones of the two tested composite-adhesive systems. Within the composite material, there was higher MES value at the restoration occluso-axial surface with the low shrink Filtek P90 composite.
DiscussionDue to the importance of polymerization shrinkage on stresses generated within the restoration-tooth assembly, this study compared the generated stresses within an MOD restoration in human maxillary first molar due to polymerization shrinkage of low shrink silorane-based versus dimethacrylate-based resin composites. With large restorations as MOD, more stresses are expected in the remaining tooth structure but fewer stresses on restoration and restoration-tooth interface [32]. Fracture of the remaining tooth structure subsequently occurs under occlusal forces [33]. The present analysis modelled the maxillary first molar with its supporting structures. The results, however, indicated that negligibly low stresses were transmitted to the root and toothsupporting tissue. This could, therefore, support the techniques modelling the crown part only [16,19]. Furthermore, the elastic-plastic behaviour of both composites as well as their adhesive counterparts, as shown in Fig. 3, was considered in the current FEA. This assumption produced more realistic and meaningful data than other FEA studies that only assumed a linear elastic behaviour of the composite and its corresponding adhesive [34]. In the present work, shrinkage was applied incrementally with no variation in the composites’ mechanical properties as the polymerization progresses; this, however, contradicts what happen in reality. The stiffness, as indicated by the elastic modulus, of a composite, however, increased monotonically from low values at the start of polymerization to its maximum values at the end of polymerization. The stiffness cold also continues to increase after curing (i.e., dark polymerization) [35]. Accordingly, the stresses computed throughout this study could be expectedly higher than the actual ones generated clinically. To avail data relevant to such variation, however, is an extensive experimental task, and this will be considered in future work.
As expected, the low shrink dental composite system resulted in lower generated stresses (MES) within the enamel, dentin, and composite than hybrid Filtek Z250 composite system. There was no difference between the two composite systems, however, in the generated stresses within the adhesive layer. As observed from the three-point bending test, the flexure strength and modulus of the hybrid Filtek Z250 were higher than low shrink composite Filtek P90. The opposite, however, was true for the corresponding adhesive systems. This couldindicate that using a combination of rigid filling having high polymerization shrinkage with a flexible adhesive produced high stresses within the tooth structures and restoration. Accordingly, early failure would be expected with Filtek Z250 composite and it’s adhesive. Generally, the stresses generated in the three zones (enamel, dentin and composite) at the end of composite polymerization process depend mainly on several factors including the percentage of composite’s polymerization volumetric shrinkage, [14,36] the stiffness of the composite, [7,15] the stiffness of the associated adhesive, [7] the stiffness of the remaining tooth structures [18] and the size of the cavity [17]. The analyzed percentage of the volumetric shrinkage of FilteK Z250 and FilteK P90 were 0.02 and 0.012 respectively.
The percentage volumetric polymerization shrinkage of a composite represents the deformation of that composite after it is freely shrunk in the course of its 100% polymerization process ∆. The constraint imposed on the deformation of the composite as a result of its polymerization in a restored crown produces pulling forces, F, mutually acting between the composite and the adhesive and between the adhesive and its neighbouring tooth tissues. The mechanical behaviour of a restored crown can be modelled by three springs having the same force “F” acting on each. The springs represent the composite, adhesive and neighbouring tooth tissues with stiffness values respectively given as kc, ka and kt. Based on the mechanics concepts of deformable bodies, the shrinkage in a composite, ∆ can be given by the following equation.

Accordingly, ∆- F/kc, equals the deformation of the adhesive, F/ka, and the neighbouring tooth tissues, F/kt. Furthermore, the magnitude of “F” is influenced by ∆, kc, ka and kt. The lower the value of any of these parameters, the less the magnitude of “F”. Since the stiffness of a material depends on its stress-strain behaviour, geometry and size as well as the load configuration. The stiffness of any part of the above system (e.g., composite, adhesive or tooth structures) increases with: (a) an increase in the modulus of its material, (b) a decrease in its size, and (c) an increase in its relevant cross section property. With relatively large MOD restorations, low kt and high ∆ values, a relatively low stresses on restorations and restoration/tooth interface are expected. Due to the presence of high bending moment and low bending crosssectional modulus, more stresses, however, are expected on the tooth structures. This finding was in agreement with other study [32]. As also indicated in the present study, the highest MES existed at the axio-gingival line angle and cervical cavo-surface margin of the enamel and dentin for the two tested composite-adhesive systems. This was in agreement with other study [37].
Comparing the MES at 100% polymerization shrinkage with the corresponding materials properties, it was clearly evident that all tested materials except the single bond adhesive had higher ultimate strength than the MES. This finding indicated that those materials could withstand the MES without fracture, but a permanent deformation could occur since the highest MES value was higher than the yield strength of each material. As a result, of that deformation, internal stresses and then possible failure could occur when the internal stresses combined with chewing stresses. Those materials should be further checked against idealized occlusal forces simulating realistic chewing cycles, i.e., dynamic loads. On the other hand, the MES generated within single bond adhesive (75 MPa) was higher than its ultimate strength (22 MPa). This may indicate that single bond adhesive is at risk; cracks may be initiated within the adhesive as a result of the polymerization shrinkage of the composite. In service, crack propagation and potential micro-leakage may occur. In such a case, the site of that possible cracking is paramount. External cracks are more dangerous than internal cracks as they grow faster. Internal cracks require alonger time to grow and reach a surface. The MES generated within both adhesives generally exceeded the estimated bond strength of most adhesives (15-30MPa); [38] therefore debonding of the restoration-tooth interface is also expected during polymerization. Looking at the dental tissues (enamel and dentin), possible fracture could also occur as the MES generated within these two structures were expected to be higher with both conventional (645 and 113 MPa respectively) and low shrink composite (503 and 80 MPa respectively) than the maximum ultimate strength of these structures (42±12 and 62±16 MPa respectively [39]). As found in another study, MOD composite restoration could exhibit microcracking and interfacial failure due to internal stresses generated by polymerization shrinkage of composite restoration and occlusal loading [19].
As a result of the generated stresses, cracking is possible at some critical sites within the composite and adhesive, at the adhesive-composite and adhesive-tooth interfaces as well as buccal and the lingual surfaces of the enamel close to the CEJ plane. This possible cracking would be expected to be higher with Filtek Z250 composite and its adhesive; accordingly earlier failure could occur with this system than its counterpart low shrink Filtek P90 system. For instance, with low shrink composite, the stresses generated within the restoration were the highest at the occluso-axial surface. This may result in either gap formation at the tooth-restoration interface, if these stresses exceed the tensile strength of the adhesive bond, or may result in cuspal deflection or cracking of the tooth structure if the generated stresses are weaker than the tensile strength of the adhesive bond [8,12]. No differences between low shrink and conventional composite systems, however, were observed at other sites of the prepared cavity walls and margins and the adhesive layer. The results of the present work does not exclude other factors that may contribute to composite survival, such as the placement technique (incremental vs. bulk), C-factor, adhesive technique and surface qualities of composite restoration [39].
ConclusionRegardless of the higher flexure strength and modulus of Filtek Z250 than Filtek P90 low shrink composite, earlier failure with Filtek Z250 could occur. This could be attributed to the expected high possibility of cracking associated with the high polymerization shrinkage Filtek Z250. The cracking could occur at some critical sites within the restoration (composite and adhesive), at the interfaces (adhesive-composite and adhesive-tooth) as well as at the tooth surfaces (buccal and the lingual surfaces of the enamel close to the CEJ plane).
AcknowledgementThis project was funded by the Deanship of Scientific Research (DSR), King Abdulaziz University, Jeddah, under grant no (3-165-35-RG). The authors, therefore, acknowledge with thanks, DSR technical and financial support. The authors would like to acknowledge Associate Prof. Iman Ismail, Operative Dentistry Division, Biomaterials Division, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia, for providing the scan of a maxillary first molar.
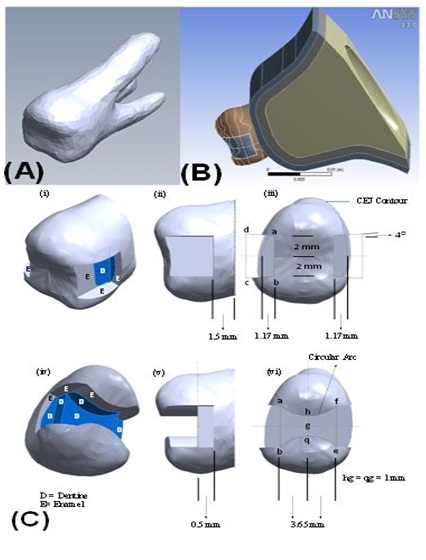
Figure 1: Geometry of the present model (A) cone beam image of the used maxillary first molar, (B) external surfaces of the present model and (C) geometry and dimensions of the cavity prepared for the modeled MOD composite restoration.
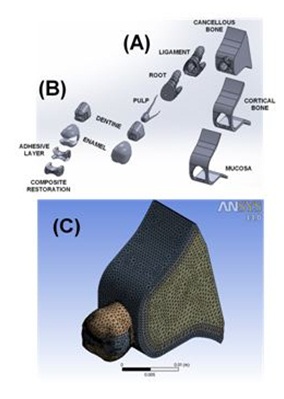
Figure 2: Idealization of the used maxillary first molar with MOD composite restoration, (A) assembly of the sound tooth parts, (B) assembly of the restored tooth and (C) analyzed finite element mesh.
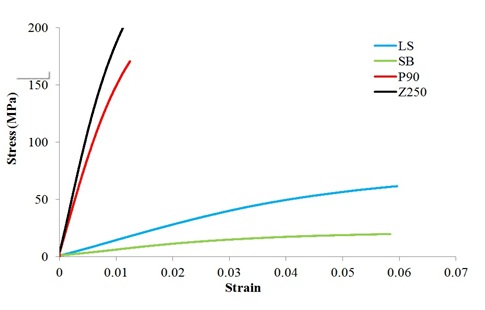
Figure 3: The bilinear stress-strain behaviour invoked in the present analysis for the two composites and their recommended adhesives; LS = P90 system adhesive; SB = Single bone universal adhesive; P90 = Filtek P90 Low shrink composite; Z250 = Filtek Z250 composite.
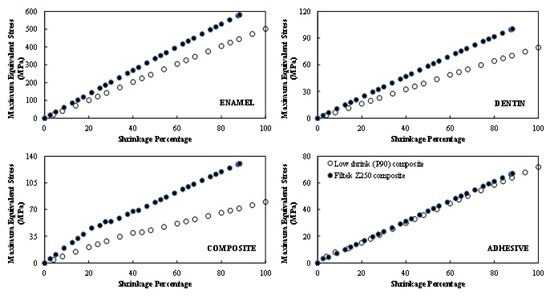
Figure 4: Development of the maximum von Mises equivalent stress within the crown regions of the analyzed first maxillary molar during the polymerization shrinkage of the used composite system; Low shrink (P90) and Filtek Z250 composites with their recommended adhesives.
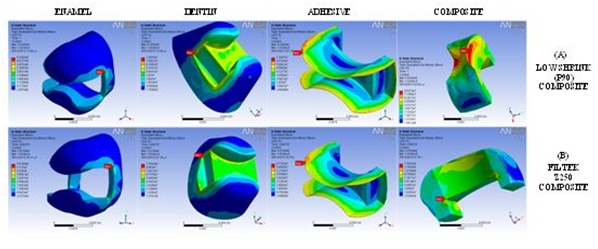
Figure 5: Computed von Mises equivalent stress fields generated within the zones of the crown of the idealized first maxillary molar due to composite polymerization shrinkage in the case of using (A) low shrink (P90) composite and (B) Filtek Z250 composite; the red arrows refer to the site of the maximum stress values.
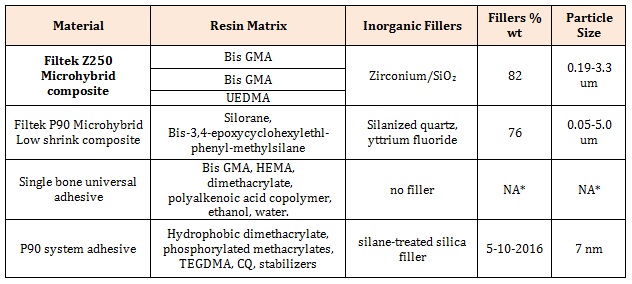
Table 1: Technical details of the used composites and associated adhesives.
* NA; not applicable
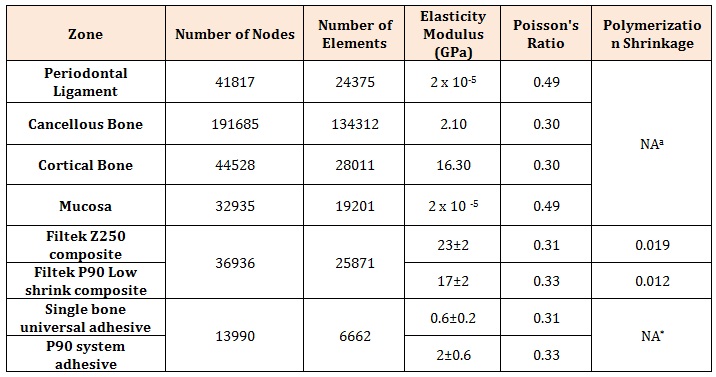
Table 2: Mesh characteristics of the different zones of the analyzed models.
* NA; not applicable